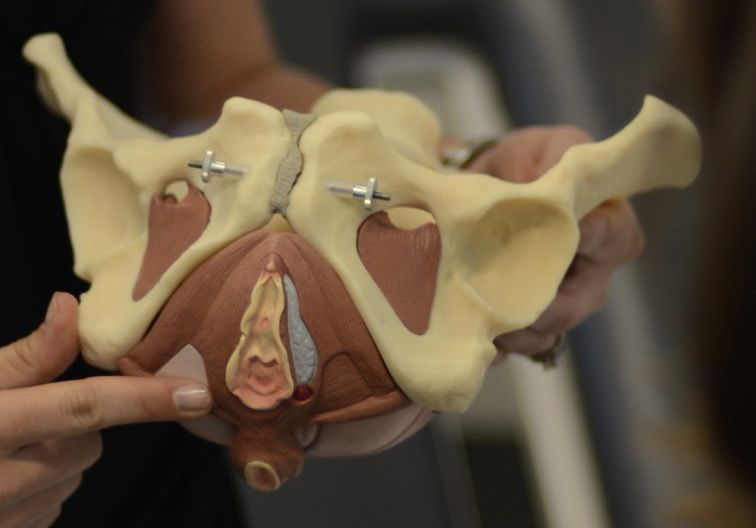
Pelvic Health Physical Therapy
Pelvic Health Physical Therapy Programs are designed to provide men and women with comprehensive services for the treatment of sensitive issues such as Urinary Incontinence, Pelvic Floor Dysfunction, and Pregnancy/Post-Partum related musculoskeletal disorders. Specially-trained physical therapists provide assessment and treatment in a supportive and private environment. A personalized treatment approach is designed to meet each patient’s needs.
Common Pelvic Health Issues Treated by Physical Therapists*
*Not available at all locations
- Abdominal, Sacral, and Rectal Pain
- Clitoral Pain
- Dyspareunia/Pain with Intercourse
- Endometriosis
- Interstitial Cystitis/Painful Bladder Syndrome
- Pelvic Organ Prolapse
- Post-prostatectomy conditions
- Pre and Post-Partum Pain
- Pudendal Neuralgia
- Tailbone Pain/Coccygodynia
- Urinary Incontinence
- Vulvodynia/Vestibulodynia
Common Pelvic Health Physical Therapy Services

Pre/Post-Partum Programs
Expand For More Info
Pregnancy can cause a number of physical changes such as weight gain, increased strain on the abdominal muscles and lumbar spine, and ligamentous laxity. These changes may cause pain that results in difficulty performing daily activities. A pregnancy and post-partum therapy program may provide:
- Assessment of posture, strength, and flexibility
- Treatment for sciatica pain
- Application of pain control modalities safe for pregnancy
- A customized exercise and manual therapy program to promote optimum musculoskeletal health and preparation of labor and delivery
- Consultation on the use of braces, supports, or assistive devices
Biofeedback Re-education for Post-Partum Patients
In women, the pelvic floor muscles are often damaged during childbirth and can lose strength as hormone levels decrease after menopause.
Biofeedback was first used by Dr. Arnold Kegel in the late 1940s to teach patients how to strengthen pelvic floor muscles (PFM). Unfortunately, most people find it difficult to identify and correctly perform Kegel exercises. The good news is that special computerized biofeedback devices can identify PFM and can assist you in controlling the performance of these muscles through visual and tactile feedback.
Some of the benefits of Biofeedback include:
- Individualized progressive treatment by trained professionals
- Awareness of pelvic muscles and achieving correct contraction/relaxation
- Improved efficiency, control, strength, endurance, conditioning & flexibility
- Pain relief

Urinary Incontinence
Expand For More Info
According to the National Association for Continence (NAFC), urinary incontinence (UI) affects 25 million Americans; 75-80% of those affected are women.
Urinary Incontinence is a social and hygienic problem for men and women of all ages. It is characterized by involuntary, uncontrollable leakage of urine. The social embarrassment experienced by those who endure the loss of bladder control can often be powerful enough to prevent them from seeking help from a healthcare provider. It is a myth that urinary incontinence is a normal part of aging and there is nothing that can be done about it.
The 2 Main Types of Urinary Incontinence
Stress Incontinence: When laughing, sneezing, coughing, or lifting a heavy object causes leakage.
Urge Incontinence & Overactive Bladder: When there is an urgency to urinate with a sudden bladder contraction, but there is the inability to get to the toilet in time.
Urinary Incontinence Treatment
In a private quiet room, each patient will have an individual evaluation that will last approximately one hour. The initial evaluation includes an internal exam if the patient is comfortable in order to properly assess the patient’s musculature and symptoms.
- Behavioral interventions (urge suppression techniques, dietary modifications, appropriate fluid intake, weight loss, habit training)
- Pelvic muscle re-training (for overactive as well as underactive pelvic floor
- Bladder training (bladder diary or scheduled voiding)
- Neuromuscular re-education (NMES) and Biofeedback

Pelvic Pain Programs
Expand For More Info
Pelvic pain can occur for many reasons. One typical cause is what is called hypertonus dysfunction or an unusual tightening of the pelvic floor muscles. This is common after a long delivery and scar tissue formation from a healing episiotomy. It can also occur from sexual abuse or when the muscles tighten to prevent the “falling out” sensation that occurs with the prolapse of the internal organs. The primary symptom is pain, but it can occur in the back, perivaginal area, lower abdomen, or thighs.
Pelvic Pain Physical Therapy
Physical therapy can help to eliminate or manage pelvic pain while restoring quality of life. This is possible through a comprehensive approach to the evaluation and treatment of the pelvic floor. In a private quiet room, the initial evaluation includes an internal exam if the patient is comfortable in order to properly assess the patient’s musculature and symptoms.
- Educational instruction
- Observation and palpation of the pelvic floor to patient’s comfort level
- Stretching and strengthening techniques
- Relaxation techniques
- Soft tissue and joint mobilization
- Modalities
- Biofeedback
- Behavior Modifications