What is pelvic organ prolapse?
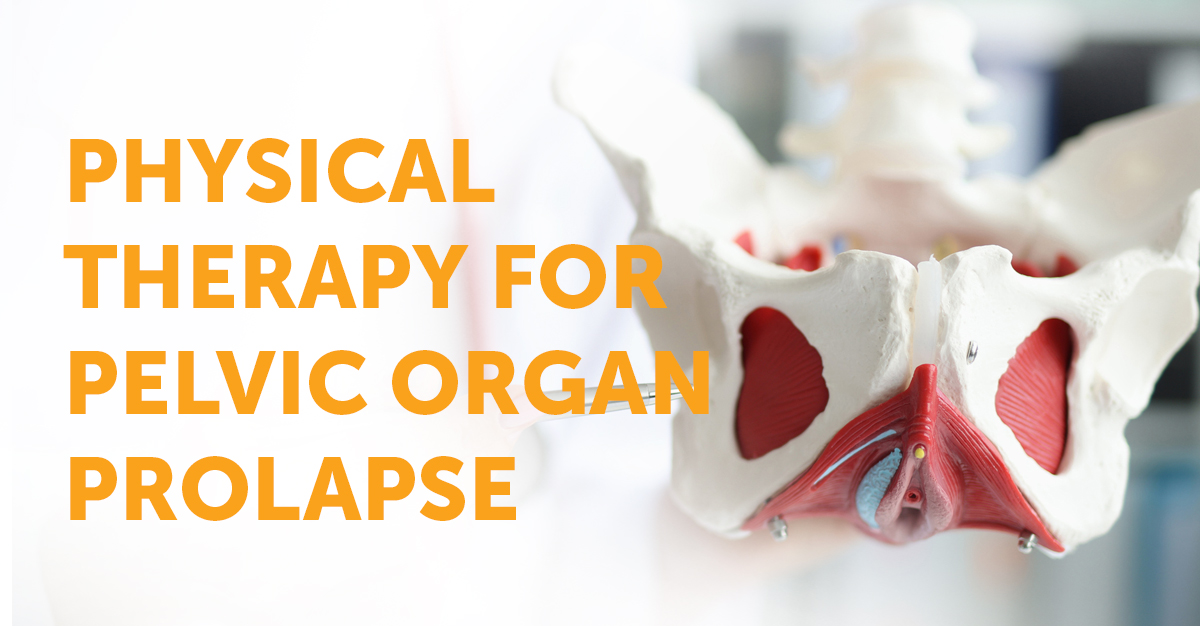
Pelvic organ prolapse, categorized as a pelvic floor disorder, affects almost 3% of women in the U.S. The pelvic floor is a group of muscles that form a hammock across the patient’s pelvic opening. These muscles and the tissues surrounding them keep the pelvic organ in place. These organs include the bladder, uterus and cervix, vagina, small bowel, and rectum. These muscles and tissues can develop problems or disorders and become more common as women age.
What is a prolapse?
Prolapse can happen when the pelvis muscles and tissues can no longer support these organs because they are weak or damaged and can cause one or more pelvic organs to drop or press into or out of the vagina.
What causes pelvic organ prolapse?
Pelvic organ prolapse is when the muscles and ligaments supporting a patient’s pelvic organs weaken, and the pelvic organs can drop lower into the pelvis, creating a bulge in the vagina (prolapse). Pelvic organ prolapse most commonly develops years after childbirth, a hysterectomy, or menopause.
Patients may experience pelvic pain for a variety of reasons. These reasons could include:
- Myofascial (muscle & fascia): Muscles of the pelvic floor can be tense, weak, shortened, or uncoordinated. Scars and fascia tightness may contribute to pain.
- Organ-related: The origin of the pain is primarily from an organ: the vulva, bladder, bowels, or uterus; Common medical diagnoses include vulvodynia, interstitial cystitis, painful bladder syndrome, endometriosis, irritable bowel syndrome, or menstrual pain.
- Nerve-related: Pudendal neuralgia is often referred to as “the carpel tunnel syndrome of the pelvic floor”. This condition is brought forth by the pudendal nerve compressing and can cause perineal or rectal pain. Injuries during childbirth, prolonged downward pressure on the pelvic floor, prolonged sitting, and bicycling are common causes of pudendal neuralgia.
What are the symptoms of a pelvic organ prolapse?
- Feeling of pressure, discomfort, aching, or fullness in the pelvis.
- Pelvic pressure that worsens with standing or coughing as the day continues.
- Trouble controlling bowels or urine, leading to leaks.
- Uncomfortable pressure during physical activity.
*Symptoms could worsen at certain times of the day, during physical activity, or after standing for a long time.
Physical Therapy for Pelvic Organ Prolapse
Pelvic Floor Physical Therapy is one of the most common treatments for pelvic organ prolapse. This specialized physical therapy relieves the symptoms of pelvic floor dysfunction and strives to help the patient’s muscles work how they should.
Pelvic floor therapy typically includes several exercises and helps the muscles relax and gain strength. A pelvic health physical therapist will work with the patient to see how strong their core muscles are and how much endurance their body has while checking the coordination of their pelvic floor muscles.
This initial assessment will help develop a plan exclusively for the patient’s body. Pelvic floor therapy plans commonly include both external and internal therapy.
Dry Needling Trigger point therapy
Trigger point dry needling is a safe, effective, and efficient treatment technique to release pain from taut bands of skeletal muscle. Trigger point dry needling uses small, thin needles to stimulate underlying myofascial trigger points, muscular and connective tissues for the management of many orthopedic conditions, both acute and chronic. By inserting a needle into the dysfunctional tissue, it often leads to a contraction of the muscle which then stimulates a release. This leads to a reduction of pain, improvements in flexibility, and restoration of normalized movement when combined with corrective exercises.
Kegels
Kegels are known for strengthening the pelvic floor as well. This exercise can help the pelvic floor muscles by contracting and relaxing them. Pelvic floor exercises such as Kegels are personalized exclusively for each patient. These personalized routines include the number of repetitions, variety of positions, time holding a pose, time relaxing, and coordination with breathing and other key muscle groups. Talk to a pelvic health physical therapist about conducting this exercise and adding it to your personalized plan.
Electrical Stimulation (ESTIM)
Pelvic health physical therapists may include ESTIM as part of treatment. Electrical stimulation works by inserting a small probe into the vagina and sending mild electrical impulses to stimulate the muscles in your pelvic floor. Electrical Stimulation can help reduce pain and muscle spasms in the pelvic region.
Biofeedback
Biofeedback, like electrical stimulation, uses a device to check the contraction of the pelvic floor muscles. It works by placing electrodes on the outside of the body or using internal probes to measure the tension and relaxation of the pelvic floor muscles. Pelvic health physical therapists use biofeedback to help guide patients as they work to strengthen or relax pelvic floor muscles.
Pelvic floor physical therapy can help reduce and eliminate symptoms of pelvic organ prolapse. Research supports using pelvic floor muscle training as an effective treatment option for patients with Grade 1 or Grade 2 pelvic organ prolapse. Once an individual’s prolapse exceeds Grade 2, they may still be able to proceed with pelvic floor therapy, but surgery is the recommended treatment for Grade 3 and Grade 4 pelvic organ prolapse.
If you find yourself in need of a pelvic health physical therapist, talk to your Ob/Gyn about what options are right for you.