For Breast Cancer Awareness Month this October, we’re getting personal and sharing stories from women we work with and love, who have gone through their own health journey with breast cancer or conditions related to breast cancer. Each story and experience is different. We hope these stories help push someone who may be on the fence regarding mammograms and care, to be proactive about their health, advocate for early detection, and support those who may be going through similar journeys.

Jenna’s Story: Breast Cancer Previvor (Testing Positive for a BRCA2 Mutation)
I found out I had a BRCA2 mutation (a breast cancer gene) in 2012. My older sister was diagnosed with breast cancer at the age of 36, which is the same age our mom was when she was diagnosed with breast cancer for the first time. I was tested with a simple blood draw by the genetics team at my clinic and it was sent to Myriad Genetics for testing. My sister who had been diagnosed with breast cancer had already gone through genetic testing and when they found a break in her BRCA2 gene, her team wanted to know if her twin sister, me (her youngest sister), and her mom also had this same break. We did.
Even prior to my genetics testing, my care team wanted me to begin surveillance 10 years younger than my mom’s first cancer diagnosis, so at age 26. The plan was just yearly mammograms. I was 26 when I found out I had a BRCA2 mutation, but still young and stupid and put off my surveillance for a bit anyway. My OB was the person who really pushed me to take it seriously and go to my appointments and screenings.
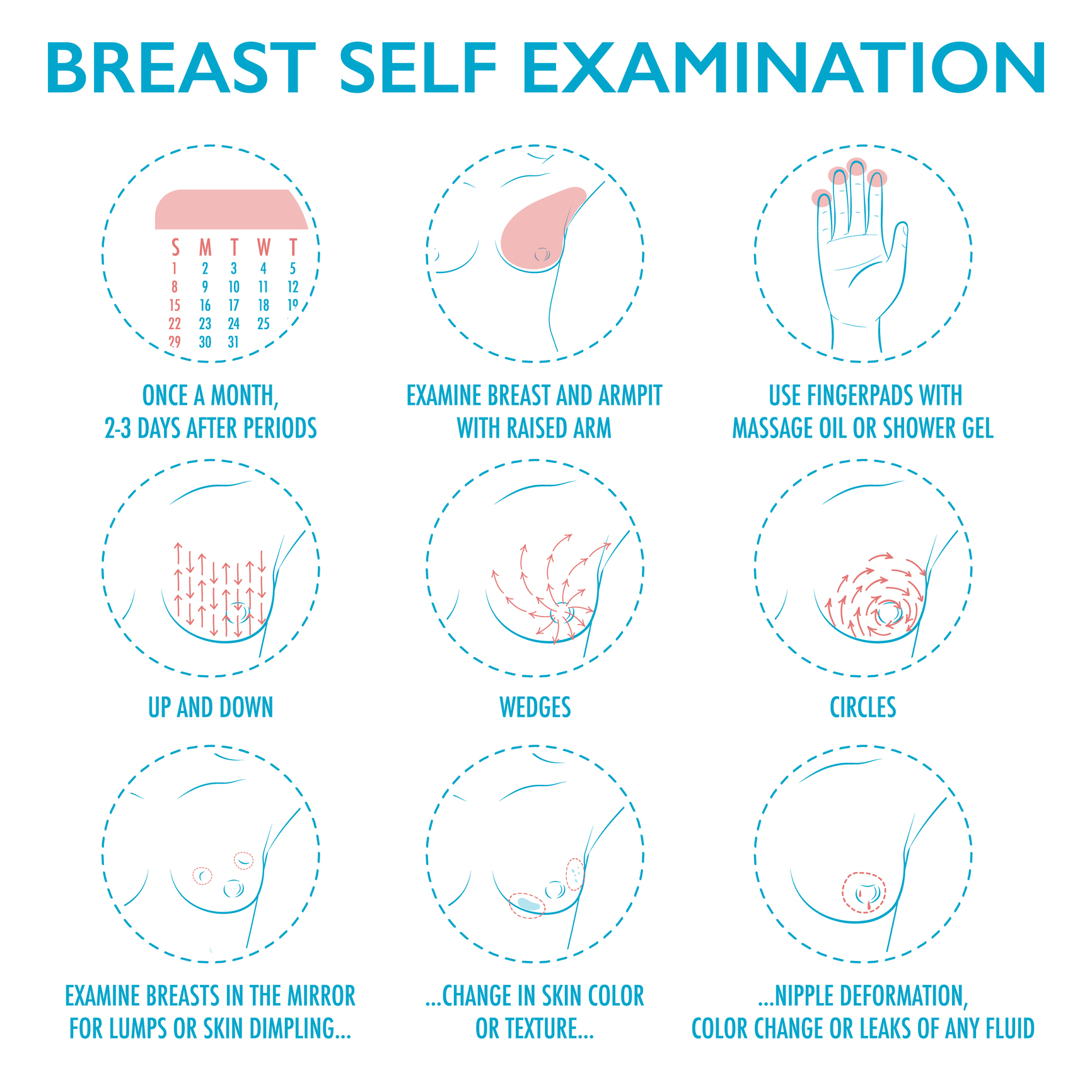
When insurance tried to deny my mammogram at such a young age, she advocated for me and contacted them on my behalf to get it approved. I never had any issue with screening after that. My surveillance was a mammogram every year, a breast MRI every year, and a visit with an oncologist once a year, so I was being screened a minimum of every 6 months. Anything that was suspicious was taken very seriously. There were a couple of times when I found a bump or something abnormal and when I called to ask about it, they scheduled me to be seen right away for an additional mammogram or an ultrasound. Thankfully, those scares were always nothing and made me feel like I was a burden, but it was great that they never made me feel that way. One was simply a blemish on my breast, but they didn’t make me feel stupid at all for calling in about it! Better safe than sorry.
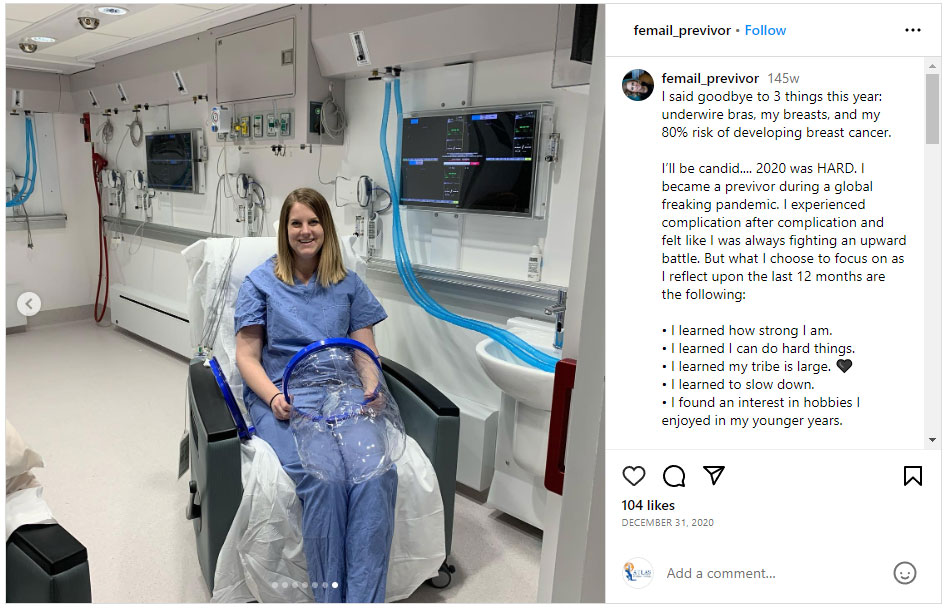
I remember trying to Google BRCA to find people like me and I couldn’t. It was maybe a month later that Angelina Jolie put out her Op-Ed about her medical decision after finding out she has a BRCA1 mutation. I began hearing about it a lot more after that, but I decided that whatever my journey, I was going to share it in hopes that it would help someone else. I now have a public figure account on Instagram where I share my journey and I have had lots of people reach out and tell me that my story has helped them. It’s the best feeling.
Choosing to Get a Mastectomy
Going back to when I found out, my now ex-husband and I took some time to think about it and talk it through, and we decided we wanted to have a family first because breastfeeding was important to both of us. I struggled to get pregnant both times, but in the fall of 2014, I welcomed my daughter Harper, and in the spring of 2019, I welcomed my son Oliver.
I felt good about my game plan because I had a solid care team who was monitoring me every 6 months. When I was pregnant, I had ultrasounds to keep up on my screening when I could not be in an MRI machine.
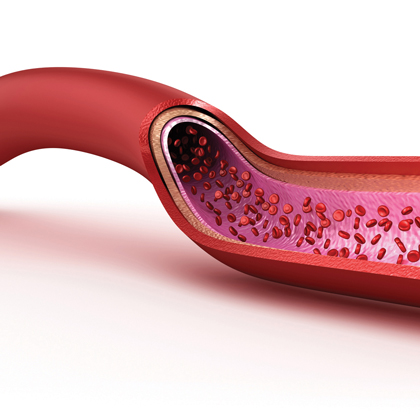
I then had a mastectomy in 2020 with a lot of complications. My plastic surgeon also helps run the wound clinic/hyperbaric department at the hospital I went to and while in surgery he actually sat me up and ran a dye through my veins to see how my blood flow looked. When he noticed that I was not getting proper blood flow to the nipples, he had me approved for hyperbaric dives through insurance starting the next morning.
Post Mastectomy Recovery
I remember being sleepy and still kind of out of it and wheeled into this department where they sized me for this weird helmet, checked my vitals, and then rolled me into a chamber room that looked like a submarine. I was the last one on that morning and there were 6 recliners in the chamber and 5 older people waiting on me. I was put into the 6th recliner, connected to leads, had pillows put under my arms and a blanket covering me up and the giant door was shut and locked.
I think I did 34 hyperbaric dives and it felt like a full-time job. It was Monday-Friday, each dive was 3 hours long and I also had to travel an hour each way to get there. I made friends with the people in the chamber with me, and almost every dive one of the older patients would pick a Western movie that was SO boring. On Wednesdays after my dives, I would see my plastic surgeon and he would evaluate my condition. Another complication was that I went directly to implant and the vertical incision under my right breast would constantly open no matter how careful I was.
Almost every week my plastic surgeon was having to cut away the edge of my skin to clean it up and re-stitch me. It got to the point where I developed a skin infection in that same breast that oral antibiotics would not clear, and I had to be admitted to the hospital for a couple of days of IV treatment (this was in February 2020). Those couple of days turned into a full week!
Shortly after my hospitalization my surgeon and I decided it was best to remove the implant on my right side and put an expander in and allow my body time to heal. Days after this surgery, the world shut down due to COVID, and I had a flat chest on the right side and a full breast on the left. I was supposed to go in for expander fills to stretch my skin once healed slowly, but those visits were flagged as unnecessary, and due to COVID restrictions, I had to wait a month before I could even begin going in for my fills. I had my expander removed and a new implant put in July 2020.
I also had fat grafting and revision surgery in August 2022 where they took some belly fat and inserted it into my breasts because you could see the ripple of the implants below my skin. This was an easy surgery.
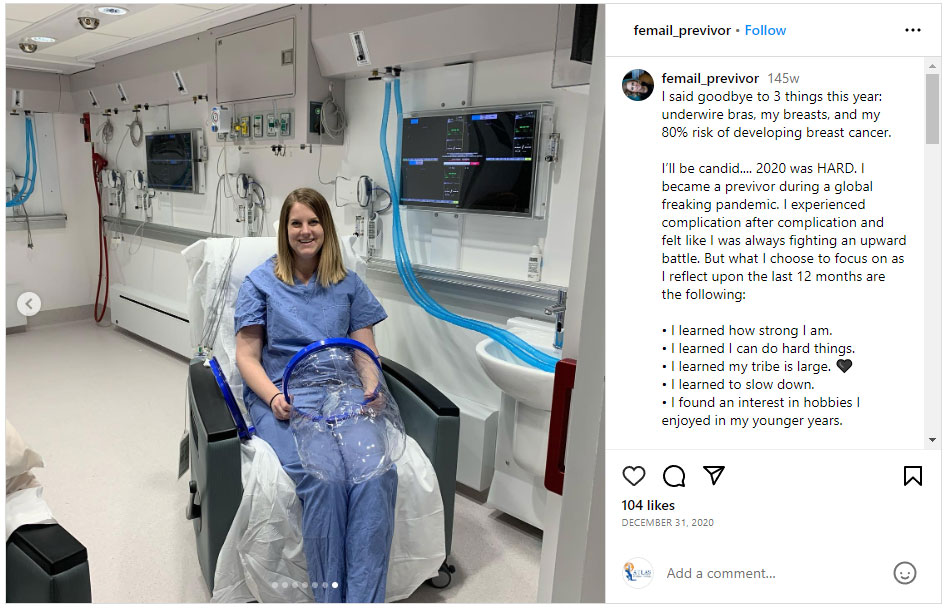
How it Feels to be a Breast Cancer Previvor
Today my health is great! My breast cancer risk is behind me now, and everything has been taken care of. My scars are there but remind me of how strong I am, and I am proud of them. My one complaint is that I still don’t have much feeling in my breasts which I knew was a probability. I can feel pressure, but the nerves were all damaged during my surgery.
In addition to my mastectomy, I am now 5 days post-op (September 21, 2023) from my full hysterectomy and oophorectomy to reduce my risk of ovarian cancer to 0%. I am doing very well recovering from this surgery but did have one complication (shocker!). My surgeon/OB said that I had “a lot of” endometriosis that we were unaware of prior to my surgery.
I had been struggling mentally with the hysterectomy and almost pushed it off because I was nervous about kickstarting menopause and was sad that I was never going to have the option to have another baby if I chose to. But finding out about the endometriosis felt like a sign that I did the right thing. My surgeon said had I waited, things would have gotten “stuck” and it would have been harder for her to remove everything successfully, especially the ovaries which are what would cause the ovarian cancer.
View the Full Blog Series