Fall Prevention Physical Therapy Programs Can Keep You On Your Feet!
One in every three adults 65 and older fall each year in the United States – WWW.CDC.GOV
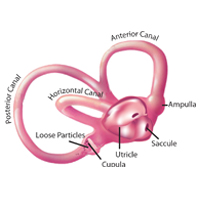
The numbers are staggering. Apparently not only does the eyesight go, but balance along with it. The two could be seen as going hand in hand since the worse your vision gets, the more likely you are to bump into or trip on something unnoticed. Fear not worried reader. Physical therapy may not improve vision, but it does improve the ability to manage and reduce the likelihood of a fall and even more importantly, a resulting hip fracture.
Fall prevention physical therapy conditioning programs offered by physical therapists are designed to increase independence with functional activities, functional mobility, and safety awareness while decreasing fall risk. Research has shown that a successful fall prevention program must be multi-dimensional. A program must address all underlying factors in addition to strength and balance. Physical therapists use valid and reliable assessments to determine all the factors affecting each individual’s fall risk. Therapy focuses on reducing the factors and decreasing fall risk. This is consistent with the protocols recommended by: The American Geriatrics Society and the American Academy of Orthopedic Surgeons’ Panel on Fall Prevention Guidelines.
THE MAIN GOALS OF THE FALL PREVENTION PHYSICAL THERAPY CONDITIONING PROGRAM ARE:
- Increase independence with Activities of Daily Living (ADLs)
- Increase independence with functional mobility
- Decrease fall risk
- Prevent future fall
- Increase safety
- Patient education
Still on the fence?
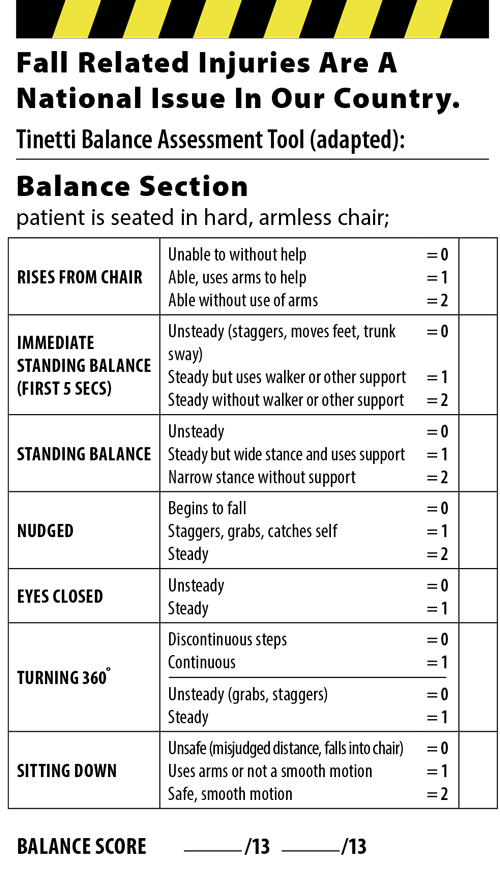
Don’t take our word for it. We have included an adapted Tinetti Balance Assessment Tool to help assess the likelihood of a fall. The Tinetti tool is the oldest clinical balance assessment tool and the widest used among older people (Yelnik, Bonan 2008). The advantages of Tinetti’s balance assessment tool are its inclusion of both balance and gait and its good inter-rater reliability and excellent sensitivity. (You can read more at the US National Library of Medicine).
Once you have taken your test – ask your physical therapist to go over the results and what options are available to decrease the risk of falls. Find your PT HERE!
For more information about balance and fall prevention click the links below: