If you think you are “too old” to do strength training exercises, think again! With proper guidance and support, you can benefit from a program of regular strength-training exercises.
Sarcopenia is the loss of muscle and strength often seen in older adults. Although many questions remain about muscle loss and aging, one thing is certain: strength-training exercises can help reduce these effects. Even small changes in muscle size can make a big difference in strength, especially in people who have already lost a lot of muscle.
BENEFITS
According to the North American Spine Society, strength training can provide the following benefits in older adults:
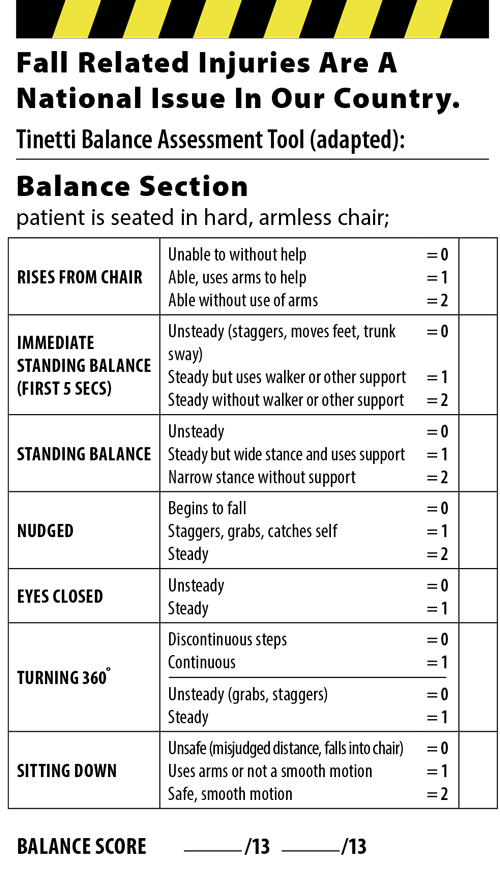
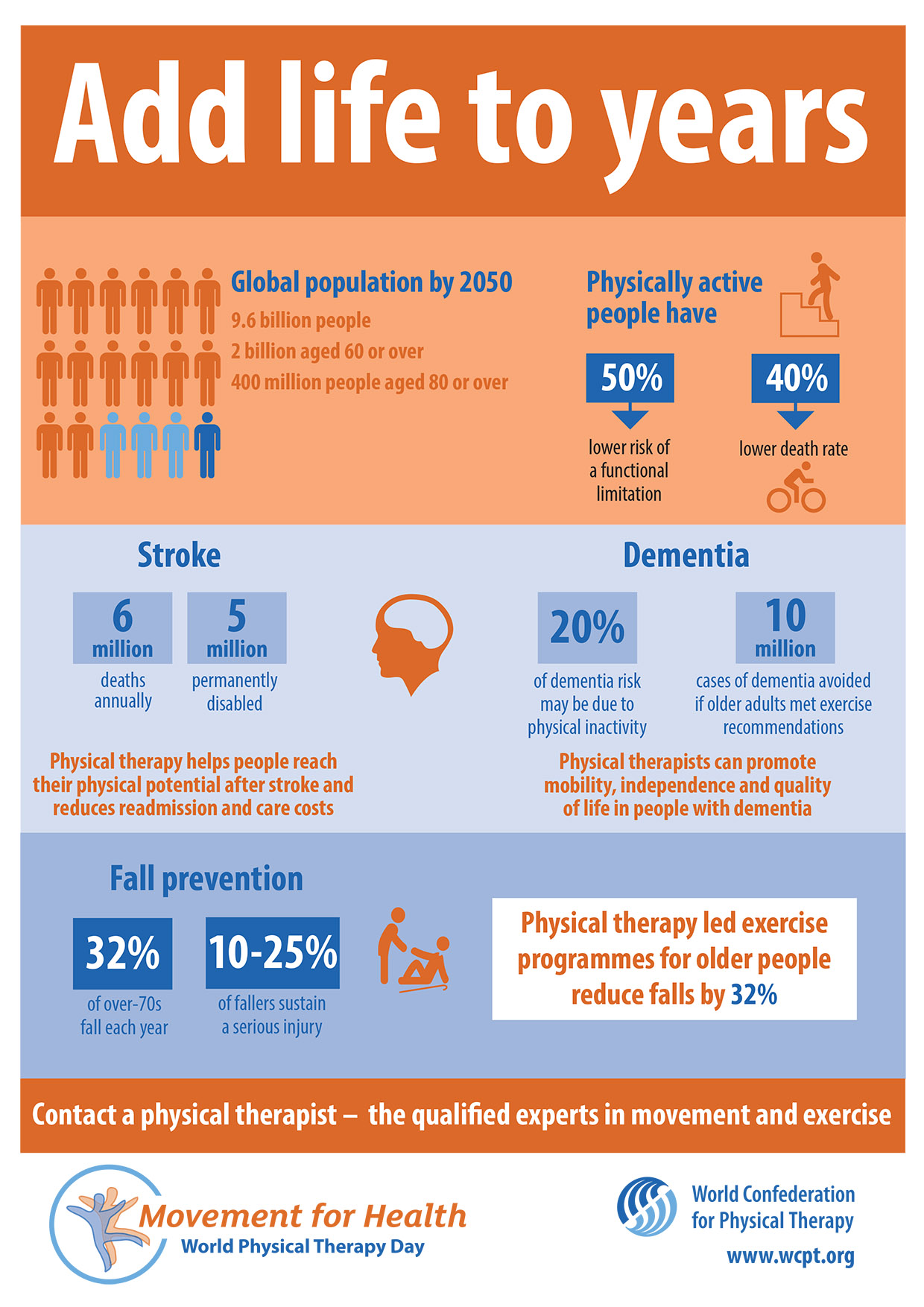
- Better balance and, consequently, reduced risk of falls
- Quicker responses, which may also play a role in preventing falls
- Reduced risk of osteoporosis (weakening of the bones)
- Improved quality of life
- Improved mental alertness
EXAMPLES OF STRENGTH-TRAINING EXERCISES
You can increase your strength by regularly using any of the following:
- Weights
- Strength-training equipment
- A resistance band
HOW MUCH AND HOW OFTEN?
The National Institute on Aging recommends the following tips on how much and how often you should do strength-training exercises:
- Exercise all of your major muscle groups at least twice a week.
- Do not do strength exercises of the same muscle group 2 days in a row.
- Depending on your condition, you might need to start out using as little as 1 or 2 pounds of weight, or no weight at all.
- Use a minimum of weight the first week, then gradually add weight. Starting out with weights that are too heavy can cause injuries.
- When doing a strength exercise, do 10-15 repetitions in a row.
- Take 3 seconds to lift or push a weight into place; hold the position for 1 second, and take another 3 seconds to lower the weight. Do not let the weight drop; lowering it slowly is important.
- Gradually increase the amount of weight to benefit from strength exercises. When you can do 2 sets of 10-15 repetitions, then you can increase the amount of weight on your next session.
- It should feel somewhere between hard and very hard for you to lift or push the weight. If you cannot lift or push a weight 8 times in a row, then it is too heavy for you. Reduce the amount of weight. If you can lift a weight more than 15 times in a row, it is too light for you. Increase the amount of weight. Do not increase more than 5% for all upper body and 10% for lower body exercises.
SAFETY TIPS
- Talk to your doctor or a physical therapist before engaging in a new exercise program.
- Breathe normally while exercising. Holding your breath (known as Valsalva maneuver) while straining can cause your blood pressure to go up. This is especially true for people with cardiovascular disease.
- If you have had a hip repair or replacement, check with your surgeon before doing lower body exercises.
- Avoid jerking or thrusting weights into position. This can cause injuries. Use smooth, steady movements.
- Avoid locking the joints in your arms and legs in a straightened position.
- Breathe out as you lift or push, and breathe in as you relax.
- Muscle soreness lasting up to a few days and slight fatigue are normal after muscle-building exercises, but exhaustion, sore joints, and unpleasant muscle pulling are not. The latter symptoms may mean you are overdoing it.
- None of the exercises you do should cause pain. The range within which you move your arms and legs should never hurt.
Looking for a physical therapist to help start your strengthening program?
Strength Training Routine for Beginners
Strength exercises can help increase your strength when performed on a regular basis. Here are some examples from the National Institute of Aging:
Wrist Curl
This exercise strengthens the wrists.
- Put your forearm on the arm of a chair. Your hand should be over the edge.
- Hold the weight with your palm facing upward.
- Bend your wrist up and down.
- Do this 10-15 times.
- Repeat with the other hand.
- Do this 10-15 more times with each hand.
Side Arm Raise
This exercise strengthens shoulder muscles.
- Sit in an armless chair with your back supported by the back of chair.
- Keep your feet flat on the floor and even with your shoulders.
- Hold hand weights straight down at your sides, with palms facing inward.
- Raise both arms to your side, shoulder height.
- Hold the position for one second.
- Slowly lower your arms to your sides. Pause.
- Repeat 10-15 times.
- Rest; then do another set of 10-15 repetitions.
Chair Stand
This exercise strengthens muscles in your abdomen and thighs. Your goal is to do this exercise without using your hands as you become stronger.
- Sit toward the front of a chair, knees bent, feet flat on the floor.
- Cross your hands over your chest and lean back in a half-reclining position. Keep your back and shoulders straight throughout the exercise.
- Raise your upper body forward until you are sitting upright, using your hands as little as possible (or not at all, if you can).
- Extend your arms outward so they are parallel to the floor. Slowly stand up, using your hands as little as possible.
- Slowly sit back down. Pause.
- Repeat 10-15 times.
- Rest; then do another set of 10-15 repetitions.
Arm Curl
This exercise strengthens upper-arm muscles.
- Stand with your feet even with your shoulders.
- Keep your feet flat on the floor and even with your shoulders.
- Hold your hand weights straight down at your sides, with palms facing forward.
- Slowly bend one elbow, lifting weight toward your chest. (Rotate your palm to face your shoulder while lifting the weight.)
- Hold this position for one second.
- Slowly lower your arm to the starting position. Pause.
- Repeat with the other arm.
- Alternate arms until you have done 10-15 repetitions with each arm.
- Rest; then do another set of 10-15 alternating repetitions.
Toe Stand
The heel raise strengthens ankle and calf muscles. You can use ankle weights for this exercise if you are able.
- Stand straight, feet flat on the floor, holding onto a table or chair for balance.
- Slowly stand on tiptoe, as high as possible.
- Hold the position for 1 second.
- Slowly lower your heels all the way back down. Pause.
- Do the exercise 10-15 times.
- Rest; then do another set of 10-15 repetitions.
- Variation: As you become stronger, do the exercise standing on 1 leg only, alternating legs for a total of 10-15 times on each leg. Rest; then do another set of 10-15 alternating repetitions.
Knee Curl
Strengthens muscles in the back of the thigh. You can use ankle weights for this exercise if you are able.
- Stand straight holding onto a table or chair for balance.
- Slowly bend your knee as far as possible. Don’t move your upper leg at all; bend your knee only.
- Hold this position for 1 second.
- Slowly lower your foot all the way back down. Pause.
- Repeat with your other leg.
- Alternate legs until you have done 10-15 repetitions with each leg.
- Rest; then do another set of 10-15 alternating repetitions.
Front Arm Raise
Strengthens shoulder muscles.
- Stand with your feet shoulder-width apart
- Hold hand weights straight down at your sides, with palms facing backward.
- Raise both arms in front of you to shoulder height. Do not turn your wrist.
- Hold this position for 1 second.
- Slowly lower your arms. Pause.
- Repeat 10-15 times.
- Rest; then do another set of 10-15 repetitions.
Leg Straightening
Strengthens muscles in front of the thigh and shin. You can use ankle weights for this exercise if you are able.
- Sit in a chair. Only the balls of your feet and your toes should rest on the floor. Put a rolled towel under your knees, if needed, to lift your feet. Rest your hands on your thighs or on the sides of the chair.
- Slowly extend 1 leg in front of you as straight as possible.
- Flex your foot to point toes toward the head.
- Hold this position for 1–2 seconds.
- Slowly lower your leg back down. Pause.
- Repeat with your other leg.
- Alternate legs until you have done 10-15 repetitions with each leg.
- Rest; then do another set of 10-15 alternating repetitions.
Back Leg Raise
Hip extension strengthens buttock and lower-back muscles. You can use ankle weights for this exercise if you are able.
-
- Stand 12-18 inches from a table or chair, feet slightly apart.
- Hold onto a table or chair for balance.
- Slowly lift one leg straight backwards without bending your knee, pointing your toes, or bending your upper body any farther forward.
- Hold this position for 1 second.
- Slowly lower your leg. Pause.
- Repeat with your other leg.
- Alternate legs until you have done 10-15 repetitions with each leg.
- Rest; then do another set of 10-15 alternating repetitions.
Side Leg Raise
This strengthens muscles at the sides of your hips and thighs. Use ankle weights, if you are ready.
- Stand straight, directly behind a table or chair, feet slightly apart.
- Hold onto a table or chair for balance.
- Slowly lift 1 leg 6-12 inches out to the side. Keep your back and both legs straight. Don’t point your toes outward; keep them facing forward.
- Hold this position for 1 second.
- Slowly lower your leg. Pause.
- Repeat with the other leg.
- Alternate legs until you have done 10-15 repetitions with each leg.
- Rest; then do another set of 10-15 alternating repetitions.
This information is neither intended nor implied to be a substitute for professional medical advice. Always seek the advice of your physician or other qualified health providers prior to starting any new treatment or with questions regarding a medical condition.
RESOURCES
National Institute on Aging
http://www.nia.nih.gov