Physical therapy for adults in retirement communities is common. Physical therapy programs can restore a great degree of functionality and bring independence to an elderly after he/she has sustained an impairment either from some chronic condition, injury, or illness. It also works when a person is recovering from surgery.
Physical therapy can be used to manage injury, deformity, or disease using physical methods rather than surgery or drugs. Typical methods include stretching, strengthening through exercise, and manual therapy. Today most outpatient physical therapy clinics and assisted living facilities for disabled adults would offer these as part of their services.
Under physical therapy, a trained therapist will evaluate and assess a person’s condition and accordingly devise a plan to suit their needs. The goal is to restore mobility and prevent future injuries. Treatment plans are usually long-term that keep in mind the degree of independence to which a person was accustomed and aim to bring that back.
Common Types of Physical Therapies for Seniors
Orthopedic Physical Therapy
When needing physical therapy for adults living in retirement communities, outpatient PT clinics offer an array of valuable services. Injuries related to the musculoskeletal system are treated by orthopedic physical therapists. Seniors recovering from orthopedic surgery are also ideal for undergoing this form of therapy. It aims to restore the functioning of joints, bone, muscles, ligaments, and tendons.
Seniors who have a hard time balancing or have reduced physical strength can also benefit from regular physical therapy sessions. It can help seniors in improving and maintaining better endurance and muscle tone enabling them to live more freely and independently. The goal is to decrease their risk of falling and accidental muscle/bone damage.
Patients suffering from post-intensive care syndrome can also benefit from physical therapy. Post-ICU physical therapy programs help patients get back into their daily routines and activities by working with them to reduce the effects of muscle loss and weakness.
Trained therapists who work at outpatient clinics and assisted living for adults with disabilities often create restorative therapy programs for the residents. These programs are led by nursing staff and caregivers with the specific needs of the patient in mind. The nursing staff prescribes certain exercises that improve strength and range of motion.
Geriatric Physical Therapy
The main emphasis under geriatric therapy is on the needs of the aging individual. Common conditions that receive treatment are – joint replacement, balance disorders, cancer, osteoporosis, and arthritis. Special programs are devised to improve fitness levels, reduce pain, and restore mobility to the maximum range.
Aquatic or Hydrotherapy
Aquatic therapy is beneficial for a few key reasons. Water decreases the gravity placed on weak limbs unable to bear much weight. This makes it easier for a patient to move, with less stress on joints, muscles, and bones. Physical therapists also utilize water to surround the patient’s body and help blood circulation in the legs. This can also reduce swelling in the patient’s ankles and feet. As the swelling decreases, the range of motion can increase.
Neurological Physical Therapy
This therapy is slightly different from all the other therapies in that it focuses on restoring brain health. Neurological physical therapy is best for the elderly who have neurological conditions like ALS, Dementia, or Parkinson’s. Those who have sustained some kind of brain injury can also benefit from it. A neurological physical therapist trains the patient to adapt to mobility, visual, and muscle loss impairments and balance issues to make their daily living as easy as possible.
Occupational Therapy
The focus of occupational therapy is on fine motor movements and hygiene-related tasks. Ideal candidates to receive this therapy are the elderly with arthritis or those who have suffered a stroke. These conditions can affect a person’s mobility and movement. An occupational therapist teaches ways to handle daily tasks with the least difficulty. It also focuses on incorporating adaptive equipment to help a person regain independence which eventually boosts the elderly’s body awareness and self-esteem.
Cardiopulmonary physical therapy
Cardiopulmonary therapy works best for individuals who have had a heart attack or suffer from some kind of heart condition. Common pulmonary conditions such as pulmonary fibrosis and Chronic Obstructive Pulmonary Disease can also benefit from this therapy. It helps to restore functional independence and endurance.
Speech-Language Therapy
The focus of this therapy is on the mouth and language-related concerns; and not just on speech as one may assume. Seniors who have a hard time chewing food or swallowing can benefit greatly from speech-language therapy. Additionally, seniors with short-term memory loss should also work with a speech-language therapist. The focus of this therapy is on cognitive issues, language deficit, and judgment concerns that are often a result of stroke or dementia.
Respiratory Therapy
Respiratory therapy is for seniors who struggle with breathing issues. It’s not uncommon for a common cold to sometimes turn into pneumonia in an occasional elderly. This can take a toll on the breathing quality. A respiratory therapist uses tapping and massage lessons to loosen the mucus which encourages easy breathing.
How Physical Therapy Benefits Seniors
Can manage chronic pain
Most seniors suffer from conditions like osteoporosis, arthritis; and as a result, suffer from pain almost every day. Studies tell that almost all elderly over the age of 65 have some degree of arthritis in their spine no matter whether symptoms persist or not. Physical therapy can preserve strength and joint health so that the onset of symptoms is delayed. If a person already has arthritis, via physical therapy they can learn therapeutic methods to reduce the level of pain and everyday discomfort.
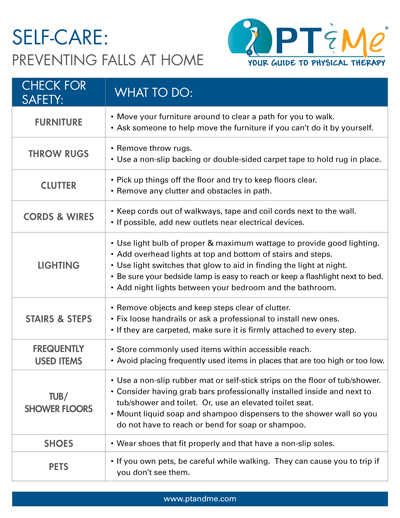
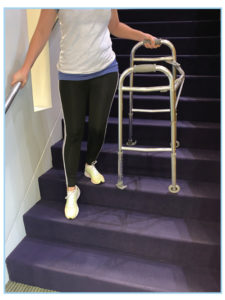
Can significantly reduce the risk of falls
Falls happen to be the leading cause of bone and head-related injuries/accidents. Also, one fall often leads to multiple falls. Physical therapy can ensure stability and strength via balancing techniques to prevent future falls.
Reduces dependence on pain medications
Physical therapy is often more effective in restoring balance and managing pain than medications prescribed by the doctor. When performed properly, it can produce almost the same kind of result in treating spine-related issues as surgery.
Reduces risk of injury
With advancing age, a person loses flexibility and muscle strength making them more prone to injuries. As part of physical therapy, a person learns several extension exercises that preserve flexibility and maintain balance to prevent falls and ensure correct posture.
Helps to regain independence and aid a healthy lifestyle
Many of the old age injuries and illnesses are due to lack of activity and mobility. Physical therapy programs incorporate various exercises to keep the elderly strong and fit. In this way, it enables them to complete everyday tasks all the while maintaining a healthy weight.
Outpatient Physical Therapy and Telehealth
Thanks to the transformation in digital technologies; seniors don’t always need to subscribe to an inpatient facility. They can work with an outpatient clinic wherein they receive physical therapy and go back to their home.
Outpatient clinics often use telehealth for physical therapy (online appointments) to work with patients that may not yet feel comfortable going into the clinic. These online telehealth appointments are more than a consultation. It is a:
- Is a full therapy visit
- Is a private, secure, and compliant way to receive care
- Sessions can be done on a computer, tablet, or phone
- Appointments are accessed on a user-friendly platform
Telehealth is a great option for seniors that are in need of care but are unable to make it into the clinic.
Final Thoughts
If you or someone you love needs physical therapy for adults living in retirement communities to recover from an illness, weakness, or injury, talk to your local physical therapist or primary care provider, and ask for more information.