What is Sciatica and the Sciatic Nerve?
The sciatic nerve is the longest and thickest nerve in the body.
It starts with five nerves in the lower back that come together and form one nerve that runs through the buttocks and down the leg. When there is inflammation of the sciatic nerve it is called sciatica. It can cause a burning or shooting pain in the buttocks or a pain that goes all the way down the leg and usually occurs only on one side.
- Pain in the back of the thigh, usually traveling below the knee; may be worse with bending, sneezing, coughing, straining, or prolonged sitting
- Numbness or weakness affecting the thigh, lower leg, ankle, or foot
- Occasionally, pain in the back or buttocks
Common Causes of Sciatica
Inflammation of the sciatic nerve because of irritation from a variety of sources, which include:
- Trauma
- A ruptured disk
- Arthritic spurs of the spine
- Spondylolisthesis (slippage of the vertebrae)
- Pressure from muscles of the pelvis (hamstring, piriformis)
- Prolonged sitting on a wallet
5 Simple Stretches to Relieve Sciatica Pain:
Pigeon Pose (Reclining)

This is a great pose for opening the hips and stretching the back (this is also used in yoga).
1. Begin by lying on your back. Bring one of your legs upward, to a right angle. Lock both of your hands behind your thigh.
2. Bring up your other leg, placing the ankle on top of the opposite knee.
3. Hold the position. This helps stretch the piriformis muscle, which is often a cause of sciatic pain.
4. Switch legs and repeat the exercise.
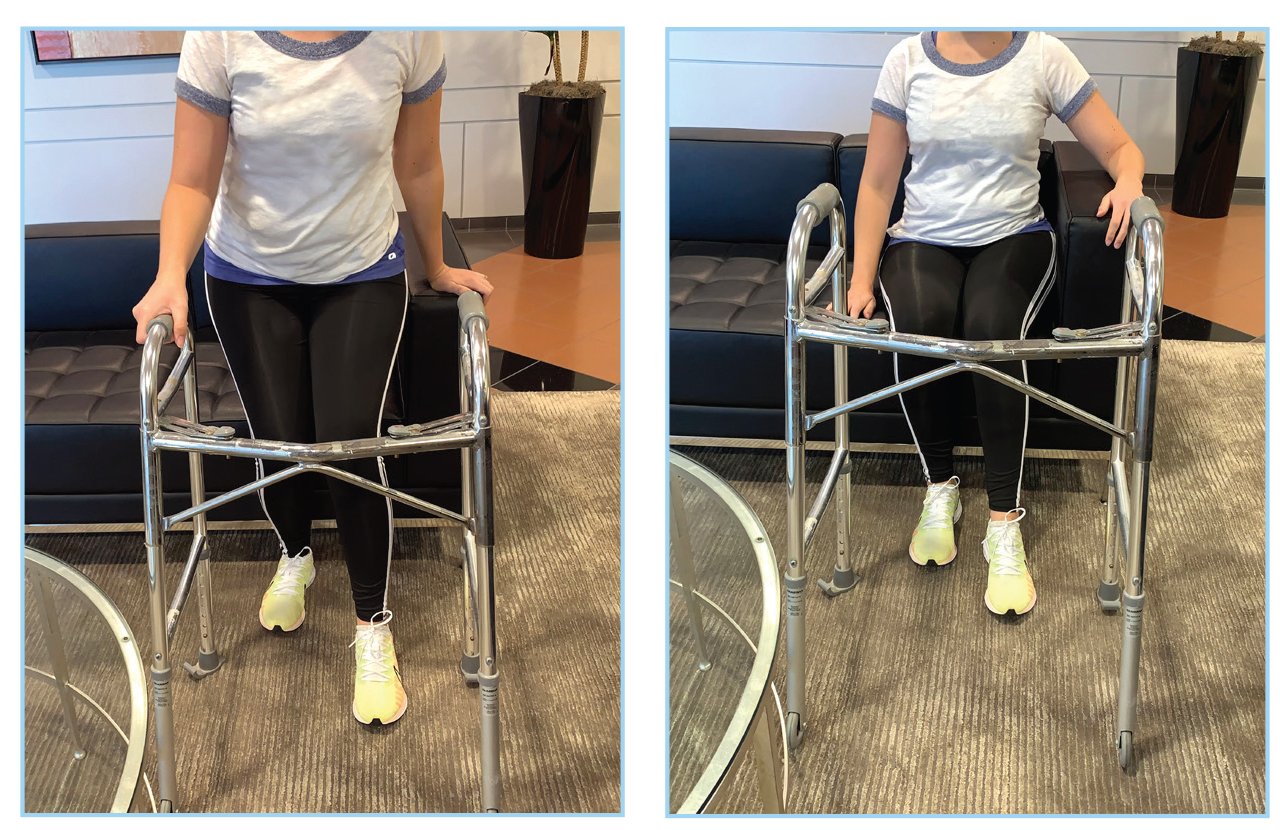
Pigeon Pose (Sitting in Chair)

This exercise is recommended if you can easily perform the pigeon pose. Try it out!
1. Sit on a stool or chair, with your legs directly in front of you.
2. Bend your right leg. Put the ankle on top of your left knee.
3. Lean forward, pushing your upper body towards your thighs.
4. Hold this position for 15-30 seconds to stretch out the muscle in the lower back and glutes.
5. Repeat on the other side.
Knees To Opposite Shoulder

This stretch offers sciatica pain relief by stretching and loosening both the piriformis and gluteal muscles.
1. Begin by lying on your back, and extending your legs.
2. Bend your right leg gently, clasping your opposite hand around the knee.
3. Pull the right leg across your body towards the opposite shoulder, holding it for up to 30 seconds. Pull only hard enough to feel a stretch – if you feel pain, reduce the force you’re using.
4. Push your knee down, returning to the starting position.
5. Repeat for a total of 3 reps, alternating each leg.
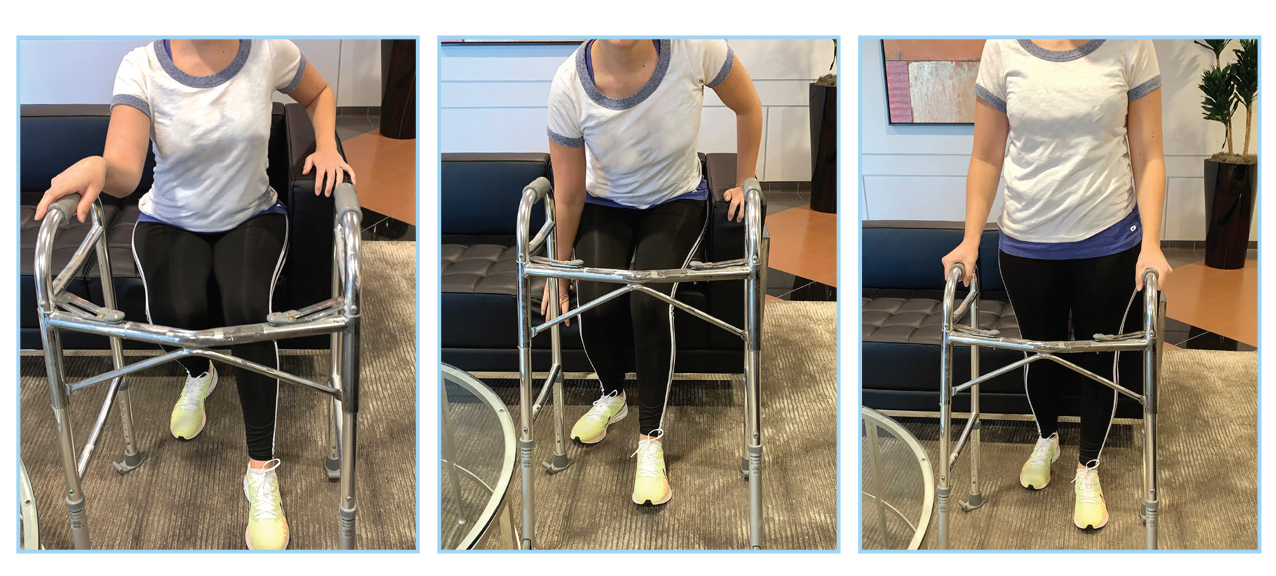
Sitting Spinal Stretch

This stretch helps relieve back pain and decompress the spine. It’s quite simple!
1. Sit on the ground in a neutral position, with your legs stretched outward.
2. Bend your right knee until you put your foot flat on the floor, past your opposite knee.
3. Place your left elbow on the right knee. Gently turn your body toward the right, flexing the spine.
4. Hold the position for 3 seconds and repeat for 3 reps on either side.
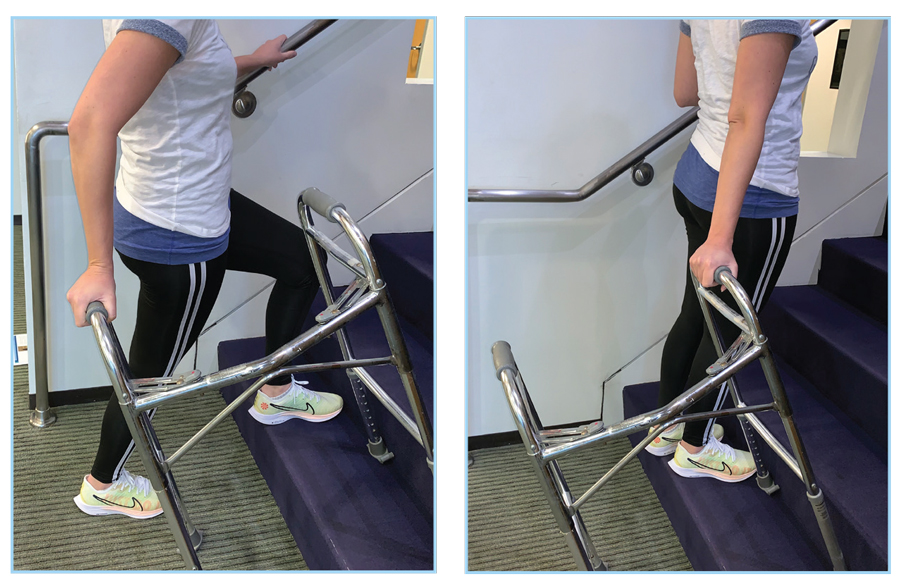
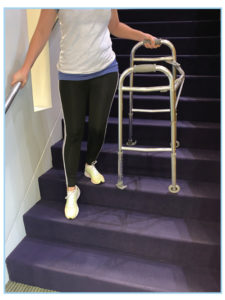
Standing Hamstring Stretch

This stretch helps relieve hamstring tightness caused by sciatica.
1. Find a flat, elevated surface such as a bench or a chair that’s at (or below) hip level. Place your right foot on this surface.
2. Keep your leg and toes straight. Bend your body forward, towards your foot, like you’re trying to touch your toes. The deeper you bend, the more intense the stretch.
3. Push the hip of your raised leg downward. Hold for 30 seconds and repeat on the opposite side.
There is no one-size-fits-all exercise for sciatic nerve pain. Never force yourself through an exercise that doesn’t feel right. Instead, focus on finding the ones that work for you! As you improve, you may be able to do some movements that didn’t work at first. Anyone experiencing pain for more than a month could benefit from seeing a physical therapist. Physical therapy and exercise help strengthen and mobilize tissues in the lower back, pelvis, abdomen, buttocks, and thighs. Commitment and frequency are important attributes of a successful treatment outcome when using physical therapy and exercise for sciatica.

Resources
Special thanks to North Lake Physical Therapy in Portland, OR for posing for our stretches!
https://www.healthline.com/health/back-pain/sciatic-stretches#What-is-the-sciatic-nerve?
https://www.webmd.com/pain-management/sciatica-exercises-pain-relief
https://www.movementforlife.com/articles/physical-therapy-sciatica-5-stretches-pain-relief
https://www.suburbanortho.com/wp-content/uploads/2017/03/Sciatica.pdf