What is Bursitis and What Causes it?
Aching, inflamed, and painful joints can often be mistaken for arthritis, but what might really be happening in your body is a case of bursitis. Although bursitis does result in joint pain, it is a condition that concerns the bursae within the joints. In our body, there are 160 tiny, slippery fluid-filled sacs called “bursa” that allow our joints to move in a smooth fashion, by providing a thin cushion and reducing friction between bones, tendons, muscles, and skin surfaces.
Although there are bursae found all over the body, the major ones are found near large joints such as the elbows, hips, knees, and shoulders. Joints with higher ranges of motion typically see the most bursitis damage leading to inflammation from repetitive use or pressure. Bursitis is the result of an inflammation of the bursae, and once these sacs become inflamed, there’s more friction between the bone and the muscles moving around, making the problem worse.
Bursitis can be caused by excessive pressure and repetitive movement. As a result, the shoulders, knees, and elbows are the most affected parts of the body. Another cause of bursitis is traumatic injury, since the bursae no longer fits in the small space between the bone and muscle or tendon.
Bursitis Symptoms to Look For:
- Feel achy or stiff
- Swelling
- Dull pain with occasional sharp pain
- Painful to the touch
- Pain (increases with movement or pressure)
How Do I Treat Bursitis?
Home treatment is often enough to reduce pain and let the bursa heal. Physical therapists can also help strengthen the muscles around your joints and relieve pain.
What do I do if I have bursitis?
- Rest the affected area. Avoid any activity or direct pressure that may cause pain.
- Apply ice or cold packs as soon as you notice pain in your muscles or near a joint. Apply ice 10 to 15 minutes at a time, as often as twice an hour, for 3 days (72 hours). You can try heat, or alternating heat and ice, after the first 72 hours.
- Use pain relievers. To reduce pain and inflammation, use nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen or naproxen. NSAIDs come in pills and also in a cream that you rub over the sore area. Acetaminophen (such as Tylenol) can also help with pain. Don’t rely on medicine to relieve pain so that you can keep overusing the joint.
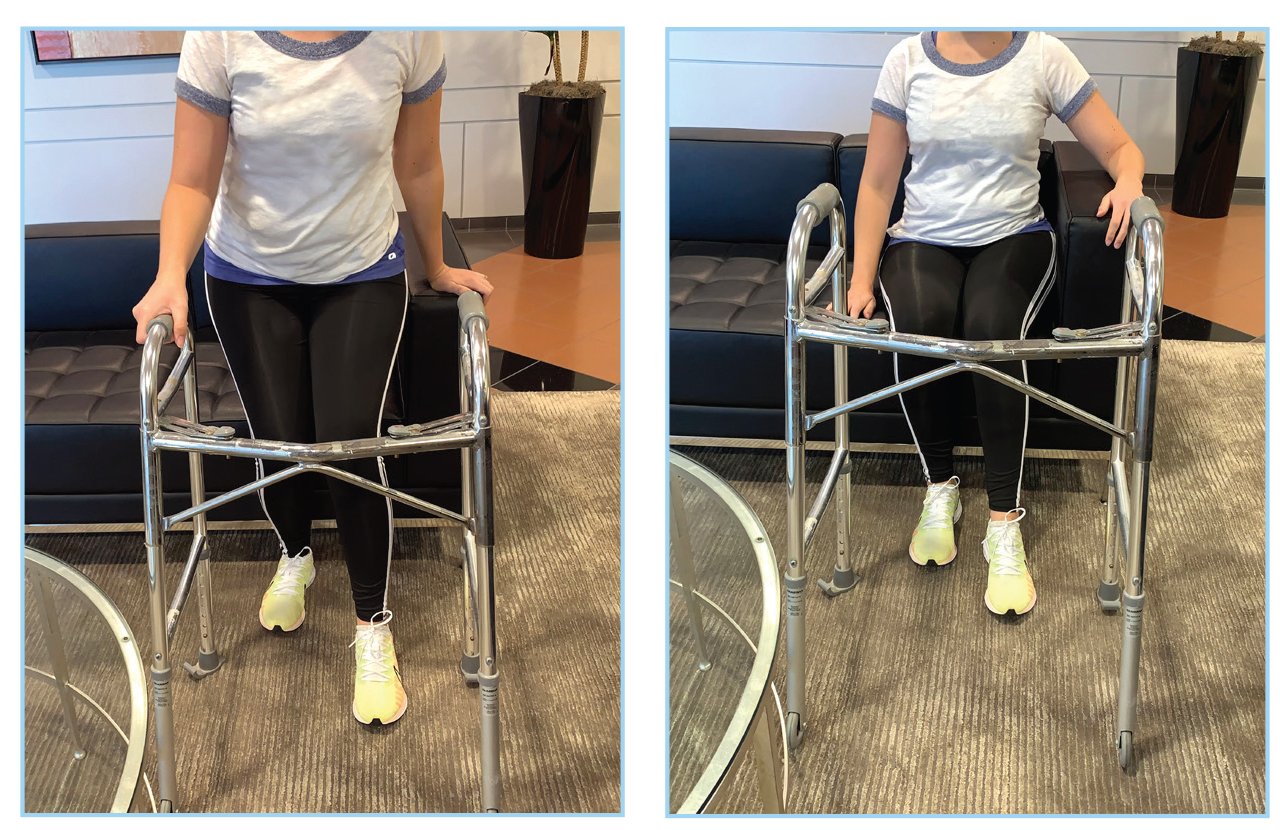
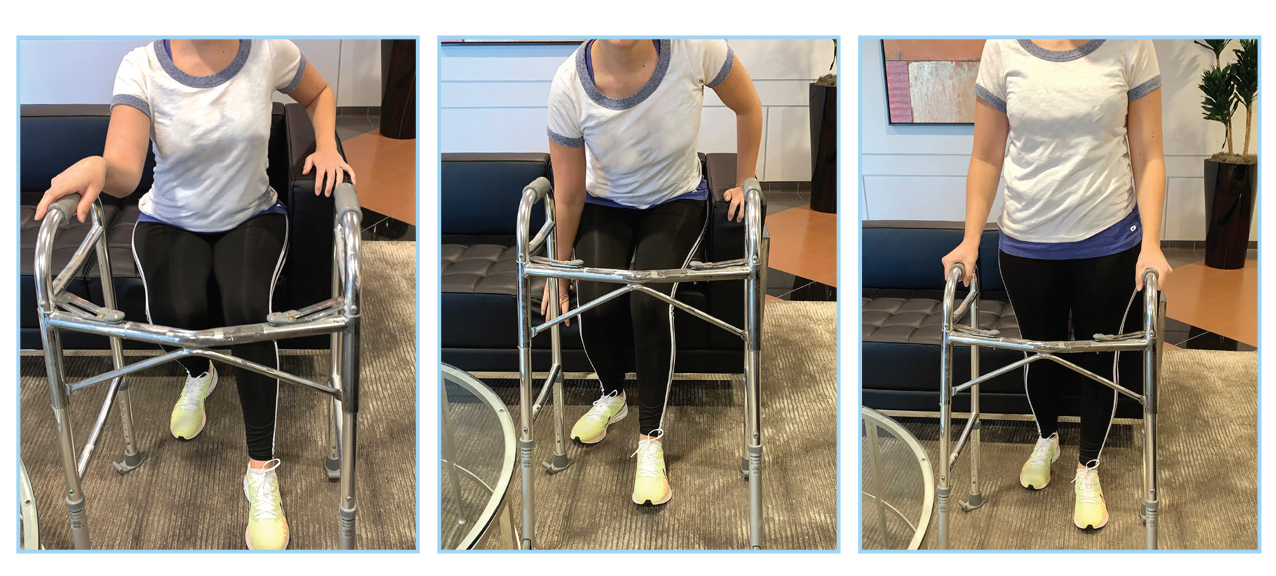
- Do range-of-motion exercises each day. If your bursitis is in or near a joint, gently move the joint through its full range of motion, even during the time that you are resting the joint area. This will prevent stiffness. As the pain goes away, add other exercises to strengthen the muscles around your joint.
- Avoid tobacco smoke. Smoking delays wound and tissue healing.
Physical Therapy treatment for Bursitis:
Your physical therapist also will perform an evaluation to determine the likelihood that you have bursitis. The time it takes to heal the condition varies, but results can often be achieved in 2 to 8 weeks when a proper stretching and strengthening program is implemented. Contact your physical therapist today to help you get on a healing & regenerative program.
The Risks of Not Treating Bursitis:
If you don’t treat this condition and develop a severe case of bursitis, your doctor may use a needle to remove extra fluid from the bursa. You might wear a pressure bandage on the area. Your doctor may also give you a shot of medicine to reduce swelling. Some people need surgery to drain or remove the bursa. Sometimes the fluid in the bursa can get infected. If this happens, you may need antibiotics.
Preventing Bursitis:
While not all types of bursitis can be prevented, you can reduce your risk and the severity of flare-ups by changing the way you do specific tasks. Examples include:
- Using kneeling pads. Use some type of padding to reduce the pressure on your knees if your job or hobby requires a lot of kneeling.
- Lifting properly. Bend your knees when you lift. Failing to do so puts extra stress on the bursae in your hips.
- Wheeling heavy loads. Carrying heavy loads puts stress on the bursae in your shoulders. Use a dolly or a wheeled cart instead.
- Taking frequent breaks. Alternate repetitive tasks with rest or other activities.
- Maintaining a healthy weight. Being overweight places more stress on your joints.
- Strengthening your muscles can help protect your affected joint.
- Warming-up and stretching before strenuous activities to protect your joints from injury.
Sources:
https://www.mayoclinic.org/diseases-conditions/bursitis/symptoms-causes/syc-20353242
https://stanfordhealthcare.org/medical-conditions/bones-joints-and-muscles/bursitis/treatments.html
https://therapydiadenver.com/resources/bursitis-pain-treatment/