It’s that time of year again. Time to exchange snow shovels and winter boots for gardening tools and watering cans. While the warmer weather brings on a new sense of happiness and energy, we need to remember to use proper body mechanics and follow general safety to avoid muscle aches and potentially serious injuries. The number one injury associated with gardening is low back pain. If you have experienced a recent injury or pain, we can help you recover.
Here are a few tips to make your gardening experience more enjoyable and less painful.
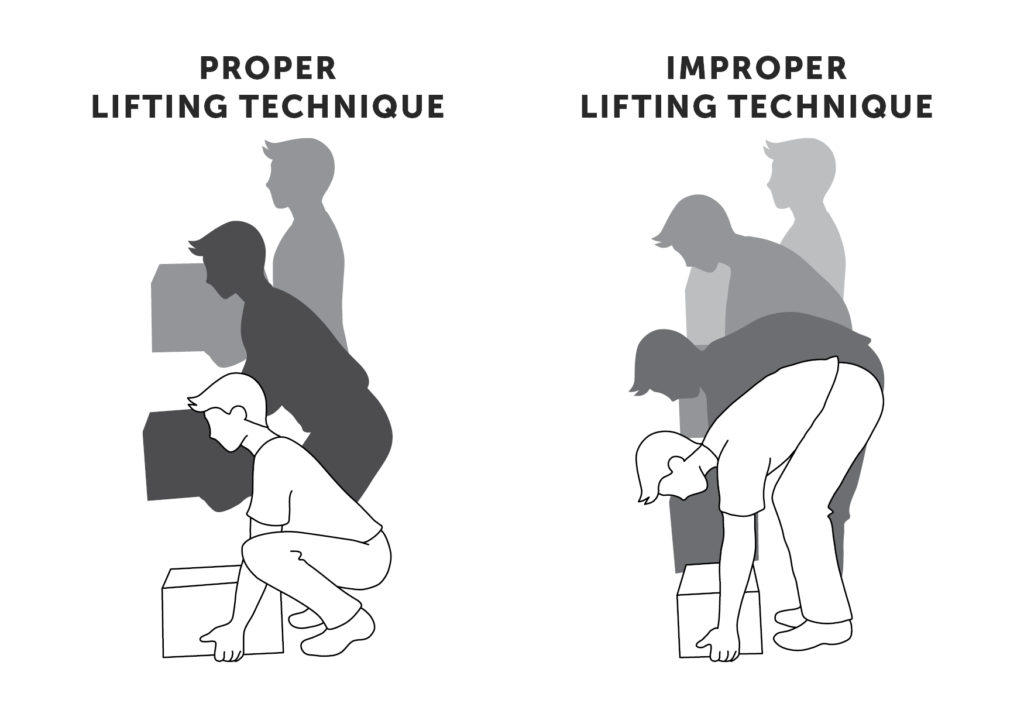
LIFTING:
Lifting heavy objects such as bags of soil, planters, and mulch improperly can lead to low back strains and/or sciatic pain. Other options include moving half of the soil/mulch to a separate pot before lifting the bag or planting into smaller pots that are easier to maneuver. Using a garden cart or wheelbarrow can also assist with moving heavy gardening materials. Remember to lift with your legs, avoid simultaneous lifting and twisting and keep heavier objects close to your body to avoid injury.
PLANTING:
Prepping the soil can also be a difficult and tedious task requiring prolonged forward bending and frequent changes in position. Try prepping the planting bed by using long-handled gardening tools. Once the soil is ready, plant from a kneeling position using either a kneeling stool or a cushion. Remember to avoid twisting the spine. Those with known chronic low back pain may want to consider planting into pots, flower boxes, or raised flower beds to avoid further injury.
WEEDING:
Most people dislike weeding their gardens and flower beds. Options to reduce the need to do so include using plants as ground cover or using mulch in your flower beds to minimize weed growth. If using a weed spray, look for bottles that have a sprayer hose to allow you to stand upright while treating your problem areas. Depending upon your fitness and capability levels, we have 3 ways to pull out weeds without injuring your back. No matter which option you choose, you need to: Stretch before you get started, Take breaks, and Never twist your back. Only work in the area directly in front of you.
MOWING THE LAWN:
Another task that most people find tedious. When able, use an electric start mower. The action of pulling a cord to start your mower is the most common cause of low back injuries. If you must use a pull start mower, remember to bend at your knees and maintain the natural curve of your spine while reaching for the cord. Make sure you tighten your abdominal muscles just before pulling the cord in order to support your spine. If using a push mower, remember to maintain a proper upright posture and take breaks as needed.
Remember to listen to your body. Take frequent breaks and change positions when you experience aching, cramping, or fatigue. Stay hydrated and wear sunscreen. If you do happen to experience low back pain or any other injury, remember to contact your physical therapist. They can help alleviate your symptoms and educate you on proper body mechanics.
GARDENING STRETCHES
Stretching before you start gardening can help you from experiencing pain later. Here are some stretching techniques to help get you started!

1.) Fold your hands together and turn your palms away from your body, but this time extend your arms overhead. You should feel the stretch in your upper torso and shoulders to your hand. Hold for 10 seconds and repeat eight times.

2.) Place your hand just above the back of the elbow and gently push your elbow across your chest toward the opposite shoulder. This is a stretch for the upper back and shoulder. Stretch both the right and left arms. Hold for 10 seconds and repeat eight times.

3.) Raise one arm overhead. Bend the elbow. Place the opposite hand on the bent elbow and gently push the elbow back further. This is a stretch for the triceps. Stretch both the right and left arms. Hold for 10 seconds and repeat eight times.
4.) Extend an arm in front of you, making sure the elbow is completely straight. With your palm down, take the opposite hand and bend in the wrist downward. Then turn the palm up, and stretch the wrist backward. This stretches the forearm and wrist muscles. Hold for 10 seconds and repeat eight times.
If you are experiencing pain, trust a licensed professional. Our therapists will help identify the cause of your pain and work with you to help it go away, and prevent pain and injury in the future.
The warm-up exercises were developed by professional hand therapists who are occupational and physical therapists specializing in the treatment of the hands, arms, and shoulders. These exercises and tips have been designed to supplement more commonly known gardening safety practices that concentrate only on preventing back injuries.
For more information visit: www.asht.org