Every year, millions of teenagers participate in high school sports. An injury to a high school athlete and the pressure to play can lead to decisions that may lead to additional injury with long-term effects. High school sports injuries can cause problems that require surgery as an adult, and may lead to arthritis later in life.
When a sports injury occurs, it is important to quickly seek proper treatment. To ensure the best possible recovery, athletes, coaches, and parents must follow safe guidelines for returning to the game.
Teenage athletes are injured at about the same rate as professional athletes, but because high school athletes are often still growing they are more susceptible to muscle, tendon, and growth plate injuries.
Types of High School Sports Injuries
Injuries among young athletes fall into two basic categories: overuse injuries and acute injuries. Both types include injuries to the soft tissues (muscles and ligaments) and bones.
Acute Injuries
Acute injuries are caused by a sudden trauma. Examples of trauma include collisions with obstacles on the field or between players. Common acute injuries among young athletes include contusions (bruises), sprains (a partial or complete tear of a ligament), strains (a partial or complete tear of a muscle or tendon), and fractures.
Overuse Injuries
Not all injuries are caused by a single, sudden twist, fall, or collision. Overuse injuries occur gradually over time, when an athletic activity is repeated so often, parts of the body do not have enough time to heal between playing.
Overuse injuries can affect muscles, ligaments, tendons, bones, and growth plates. For example, overhand pitching in baseball can be associated with injuries to the elbow. Swimming is often associated with injuries to the shoulder. Gymnastics and cheerleading are two common activities associated with injuries to the wrist and elbow.
Stress fractures are another common overuse injury in young athletes. Bone is in a constant state of turnover—a process called remodeling. New bone develops and replaces older bone. If an athlete’s activity is too great, the breakdown of older bone occurs rapidly, and the body cannot make new bone fast enough to replace it. As a result, the bone is weakened and stress fractures can occur—most often in the shinbone and bones of the feet.
Concussion
Concussions are mild traumatic brain injuries. They are caused by a blow to the head or body that results in the brain moving rapidly back and forth inside the skull.
Although some sports have higher instances of concussion—such as football, ice hockey, and soccer—concussions can happen in any sport or recreational activity.
Growth Plate Injuries
Growth plates are areas of developing cartilage tissue near the ends of long bones. When a child becomes full-grown, the growth plates harden into solid bone.
Because growth plates are the last portion of bones to harden (ossify), they are vulnerable to fracture. Growth plates regulate and help determine the length and shape of adult bone, therefore, injuries to the growth plate can result in disturbances to bone growth and bone deformity.
Growth plate injuries occur most often in contact sports like football or basketball and in high impact sports like gymnastics.

Treatment
Treatment will depend upon the severity of the injury, and may include a combination of physical therapy, strengthening exercises, and bracing. More serious injuries may require surgery.
Return to Play
A player’s injury must be completely healed before he or she returns to sports activity.
In case of a joint problem, the player must have no pain, no swelling, full range of motion, and normal strength.
In case of concussion, the player must have no symptoms at rest or with exercise, and should be cleared by the appropriate medical provider.
Prevention
Many high school sports injuries can be prevented through proper conditioning, training, and equipment.
High school athletes require sport specific training to prevent injury. Many injuries can be prevented with regular conditioning that begins prior to the formal sports season. Injuries often occur when athletes suddenly increase the duration, intensity, or frequency of their activity. Young athletes who are out of shape at the start of the season should gradually increase activity levels and slowly build back up to a higher fitness level.
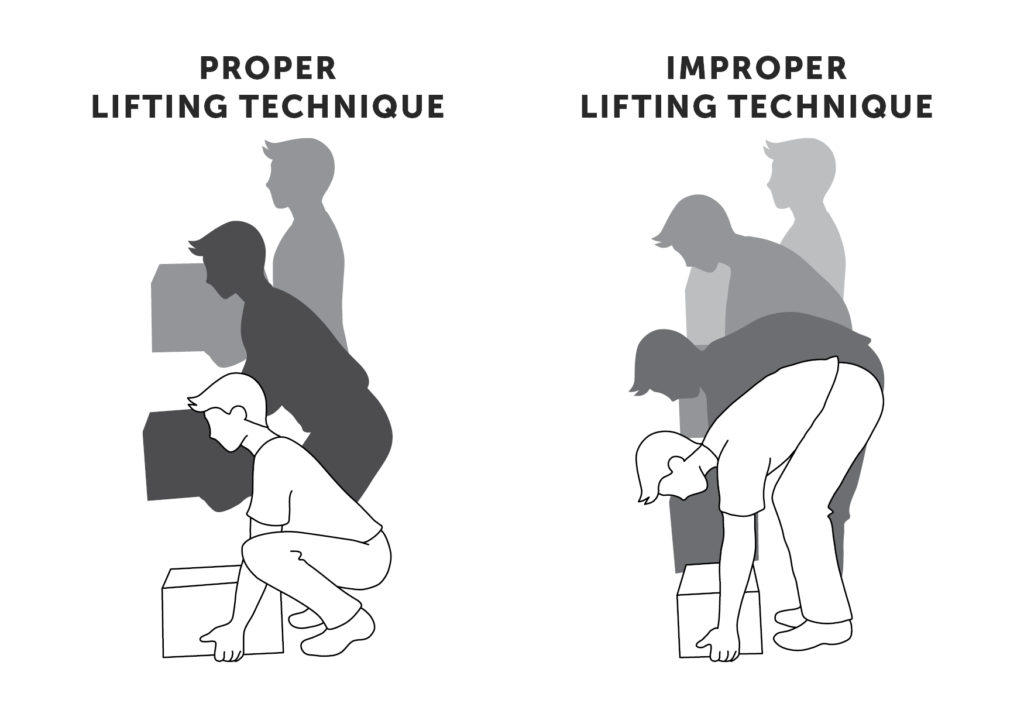
Using proper technique for the position being played is also key to preventing injury. Proper equipment—from the right shoes to safety gear—is essential. In addition, injuries can be prevented when athletes understand and follow the rules of the game, and display good sportsmanship.
Information provided by American Academy of Orthopaedic Surgeons