Isokinetic devices have had their time in the spotlight of the rehab world. Like an actor past his prime, these monstrous machines mostly sit in dark lonely corners collecting dust. Some get used regularly but only as a place for sitting and storing odds and ends. However, companies such as CSMi (Computer Sports Medicine Inc.) among others have revived this once proud and prominent piece of equipment and have applied modern technology and rehab principles to bring about a new golden age of isokinetic devices and rehab.
Historically, isokinetics was introduced in the late 1970s and hit it’s stride in the 1980s through the 90s. Various protocols were created in this time and have been researched extensively creating the body of knowledge we now have. Unfortunately, isokinetics lost favor as healthcare laws changed and the industry started the search for more low-cost treatment regimens.
ISOKINETIC DEVICES TESTING
There are now fewer therapists who know how to use the equipment and most that do are unaware of the improvements that have been made over the last twenty years. Historically, joints are measured at two or three varying speeds but only in the concentric mode of contraction. While this is still the gold standard of testing, it fails to assess the all important eccentric mode of contraction. Recently, CSMi introduced the interrupted stoke test on their machine, the Humac Norm, which allows the therapist to separate concentric and eccentric modes. Our muscles function as eccentric controllers of motion and the ability to test this provides us with a better view into the muscle’s strength and function.
There are other testing modes available as not all patients are appropriate for isokinetic testing. Isometric testing is something all therapists use daily in the form of manual muscle testing(MMT). However, this is not a precise measurement and can vary between therapists. Testing a patient isometrically on a machine is a safe, effective and precise test for your older, untrained and post-surgical patients. It provides an exact amount of torque as compared to the MMT 5-point system. Additionally, proprioception can be assessed for either velocity or joint position matching.

TREATMENT
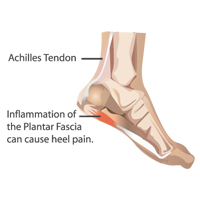
In addition to testing, isokinetic devices offer various treatment modes are where these machines show their true capability. Continuous Passive Motion can be utilized for regaining range of motion, reducing swelling and pain, reducing apprehension and muscle guarding and regaining musculotendonous mobility.
Active Assisted Programs can be utilized to regain end-range motion and multi-angle isometrics can be utilized to increase joint stability and neuromuscular control within the entire available range of motion. Also, proprioception training can be utilized to enhance positional and motion control.
Strength training with eccentric loading allows for targeted strengthening by isolating the eccentric beginning in slower speeds and progressing into deceleration training to mimic plyometric loading.
Isotonic strengthening programs are available for various purposes. One is power training which is utilized to increase concentric explosiveness. Another is used to prepare patients for an independent gym program. Finally, dynamic isotonic control training includes the ability to load the concentric and eccentric motions at different torques and utilizes games and other programs as visual feedback to the patient.
ARGUMENTS AGAINST ISOKINETICS
One argument against isokinetics concerns patellofemoral, post-op ACL and knee osteoarthritis patients. Open chain knee extension has been labeled public enemy number one for these patients and while this has been examined extensively, steps such as limiting the range of motion, using anti-shear devices and techniques, altering patient positioning and matching the appropriate treatments to the patient reduces shearing and compression, improves safety and ultimately debunks this myth.
Now, I know that critics of isokinetics will also argue that isolating muscles is not functional. That would be true if a therapist utilized these machines as the sole treatment. But by incorporating it into an eclectic approach, patient outcomes are maximized. Your lower extremity patients will still perform scapular and thoracic control exercises and you will still strengthen the core. Soft tissue work and joint mobilization will still be needed and functional training must still occur. However, if one link in the chain is weak, the entire chain will fail. Utilizing these machines throughout the course of rehab to find and isolate those weak links is what will take your patient’s recovery of function to the next level. This is true for all of your extremity patients, nit just knees. Remember, a functional movement cannot occur with a dysfunctional or unbalanced segment.
This information was written by Daniel Bodkin, PT, DPT, ATC – STAR Physical Therapy, Columbia (North), Tennessee
Established in 1997 with one clinic and one mission – to serve. Today, STAR Physical Therapy has grown to offer that direct service in more than 60 clinics, and while they’ve grown, one thing that has not changed is their commitment to you, their communities, and their employees. Their foundational mission is “To Serve.” Their commitment to the patient and physician is to provide clinicians that are “great mechanics of the human body™.” For more information click here.