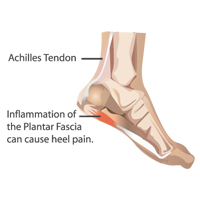
Does your foot or heel hurt with the first step in the morning? Does your foot hurt when you get up from sitting or driving for long periods of time? If the answer is yes, you may have plantar fasciitis. Plantar fasciitis is the most common type of foot pain. Plantar fasciitis is the irritation or inflammation of the plantar fascia. The plantar fascia is a thick dense connective tissue that attaches to the heel and ball of the foot. A related problem is a heel spur which is extra bone that may grow from the heel bone. This is in response to the plantar fascia being tight or inflamed, thus pulling on the heel bone.
Inflammation and microtears occur more commonly in sports that involve running, long-distance walking, dancing, tennis, basketball, and in non-athletes who spend long periods of time walking on unyielding surfaces. Patients with pes planus and heel pronation have an increased likelihood of developing plantar fasciitis because of the increased tension on the plantar fascia caused by these anatomic features. A tight gastrocnemius can result in heel pronation thereby making plantar fasciitis more likely. Cavus feet with relative rigidity also place more stress on the plantar fascia. The plantar fascia also tends to become more rigid with age making it less effective as a shock absorber and more likely to develop microtears.
Common Causes of Plantar Fasciitis:
- Too Rapid of an Increase in Exercise Program.
- Change in Lifestyle (Active to more Sedentary) Causing Sudden Weight Gain or Sedentary to Active.
- Muscle Tightness and/or Weakness.
- Poor Biomechanics (movement) at the Foot and Ankle.
- Inadequate Cushioning in Shoes or Inadequate Shoes.
- Occupation with prolonged weight bearing on Hard Surfaces.
Plantar Fasciitis Symptoms:
People with plantar fasciitis complain of searing pain at the point of the fascias insertion into the calcaneus. This pain is at its worst with the first few steps upon arising in the morning or after a sustained period of being off their feet. The plantar fascia origin is often extremely tender to palpation. Pain is also increased after long periods of walking, climbing stairs or doing toe raises.
For Plantar Fasciitis Pain Relief at Home – Try These Stretches:
Frozen Can Roll
Take a frozen food can and roll your foot forwards and back.
Towel Grab
Grab and pick up a towel or dishcloth using only your toes.
Finding Plantar Fasciitis Relief with Physical Therapy:
Physical Therapy for Plantar Fasciitis
Physical therapy evaluation generally reveals an antalgic gait pattern especially when first beginning to walk. Often foot is pronated, gastrocnemius is shortened and there is severe pain with palpation of the inferior, medial heel. Most people can experience relief in just a few sessions. However, the longer the pain remains untreated, the longer it will take to heal. It can even become so chronic in some cases other non-conservative treatments are deemed necessary. If you are experiencing symptoms similar to the ones listed earlier you may have plantar fasciitis. If you are diagnosed with plantar fasciitis physical therapy can help you resolve your pain.
Physical therapists take the time to educate each plantar fasciitis patient on how to prevent a recurrence of pain. They provide preventative stretching programs that can be done at home, instruct on what to look for when purchasing new shoes, and if necessary, help patients adapt their current lifestyle to prevent re-injury.