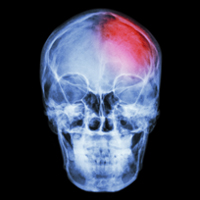
Stroke is a brain injury caused by an interruption in blood flow. It is a leading cause of death in the US, and can also cause disability, decreased quality of life and increased healthcare expenses. There are many lifestyle factors that affect you risk of stroke including diet, exercise, smoking and stress. Other lifestyle habits like long periods of standing or long work hours are also being reviewed for their impact on stroke risk.
Earlier research has suggested that long working hours may be linked to stroke, but the evidence is limited. Researchers wanted to determine if there was a possible connection between long work hours and the risk of stroke. The study, published in Lancet, found that employees who work long hours have a higher risk of stroke than those who do not.
About the Study
The systematic review of observational studies included 528,908 men and women from Europe, the U.S. and Australia who were free from history of stroke at the beginning of the study. The participants volunteered their work hours and were tracked for the development of stroke. During an average 7.2 year follow up there were 1,722 stroke-related events.
Compared to those who worked standard hours (35-40 hours/week), participants who worked 49-54 and more than 55 hours a week had an increased risk of stroke.
The effects remained apparent even when other stroke factors like age, sex and health history were accounted for.
How Does This Affect You?
A systematic review pools a large number of trials to create a larger pool of data. The larger the pool of data, the more reliable outcomes are. However, the review is only as reliable as the trials that are included. The included studies were all observational studies which means a direct cause and effect link could not be established and the studies can only show a potential link between factors.
There is a reasonable link between extra work hours and stroke since longer hours are often associated with extra stress and less relaxation time. If you have long work hours, you may want to talk to your doctor about your personal risk factors for stroke and follow other stroke prevention methods such as:
• Exercising regularly
• Maintaining a healthy weight
• Eating more fruits, vegetables and whole grains and limiting dietary salt and fat
• If you smoke, talking to your doctor about way to quit
• Increasing your consumption of fish
• Drinking alcohol in moderation
• Managing chronic medical conditions, such as high blood pressure, high cholesterol and diabetes
Rehabilitation doesn’t reverse the effects of a stroke. Its goals are to build your strength, capability and confidence so you can continue your daily activities despite the effects of your stroke.
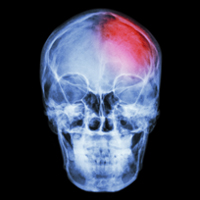
What is a Stroke?
A stroke is a disease that affects the arteries leading to and within the brain. It is the No. 5 cause of death and a leading cause of disability in the United States.
• A stroke occurs when a blood vessel that carries oxygen and nutrients to the brain is either blocked by a clot or bursts (or ruptures). When that happens, part of the brain cannot get the blood (and oxygen) it needs, so it and brain cells die.
What are the Effects of Stroke?
The brain is an extremely complex organ that controls various body functions. If a stroke occurs and blood flow can’t reach the region that controls a particular body function, that part of the body won’t work as it should. Rehabilitation is probably one of the most important phases of recovery for many stroke survivors. The effects of stroke may mean that you must change, relearn or redefine how you live. Stroke rehabilitation helps you return to independent living.
Rehabilitation doesn’t reverse the effects of a stroke. Its goals are to build your strength, capability and confidence so you can continue your daily activities despite the effects of your stroke.
What Will I Do in Rehabilitation?
What you do in rehabilitation depends on what you need to become independent. You may work to improve your independence in many areas. These include:
• Self-care skills such as feeding, grooming, bathing, toileting and dressing
• Mobility skills such as transferring, walking or self-propelling a wheelchair
• Communication skills in speech and language
• Cognitive skills such as memory or problem solving
• Social skills for interacting with other people
by Cynthia M. Johnson, MA
RESOURCES:
Family Doctor—American Academy of Family Physicians
http://familydoctor.org
American Stroke Association
http://www.strokeassociation.org
Kivimäki M, Jokela M, et al. Long working hours and risk of coronary heart disease and stroke: a systematic review and meta-analysis of published and unpublished data for 603,838 individuals. Lancet. 2015 Oct 31;386(10005):1739-1746. Available at: http://www.thelancet.com/journals/lancet/article/PIIS0140-6736%2815%2960295-1/fulltext. Accessed January 19, 2016.
Risk factors for stroke or transient ischemic attack. EBSCO DynaMed website. Available at: http://www.ebscohost.com/dynamed. Updated December 28, 2015. Accessed January 19, 2016.
Last reviewed January 2016 by Michael Woods, MD
EBSCO Information Services is fully accredited by URAC. URAC is an independent, nonprofit health care accrediting organization dedicated to promoting health care quality through accreditation, certification and commendation.