Women’s bodies and their wellness are unique. Many factors cause problems specific to women’s bodies. Physical therapists specializing in women’s health can help female patients eliminate or manage pelvic pain or problems while restoring their quality of life. Using a comprehensive approach to evaluation and treatment, women’s health physical therapy programs can provide relief for these 4 common pelvic issues:
- Pelvic floor pain or dysfunction
- Pelvic organ prolapse (POP)
- Postpartum recovery and or pain
- Urinary incontinence
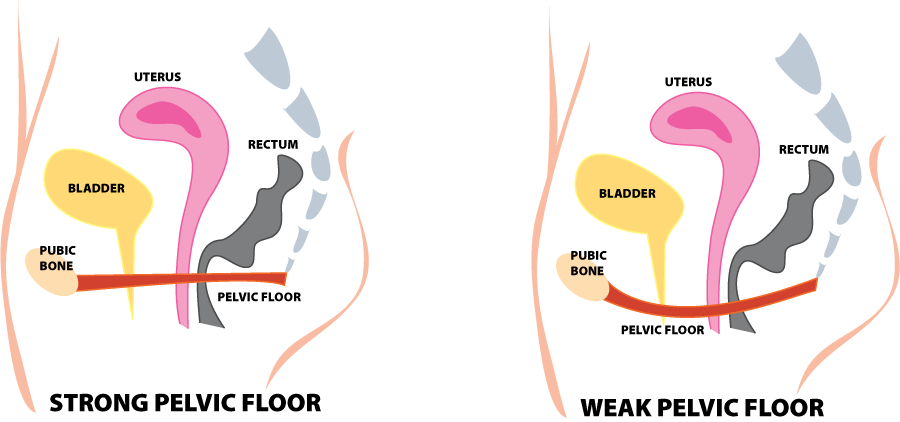
1. Pelvic Floor Pain or Dysfunction
Pelvic pain can occur for many reasons. One typical cause is what is called a hypertonus dysfunction or an unusual tightening of the pelvic floor muscles. This is common after a long delivery and scar tissue formation from a healing episiotomy. It can also occur from sexual abuse or when the muscles tighten to prevent the “falling out” sensation that occurs with the prolapse of the internal organs. The primary symptom is pain, but it can occur in the back, perivaginal area, lower abdomen, or thighs.
How physical therapy can help pelvic pain patients:
Physical therapy can help to eliminate or manage pelvic pain while restoring the quality of life. This is possible through a comprehensive approach to the evaluation and treatment of the pelvic floor.
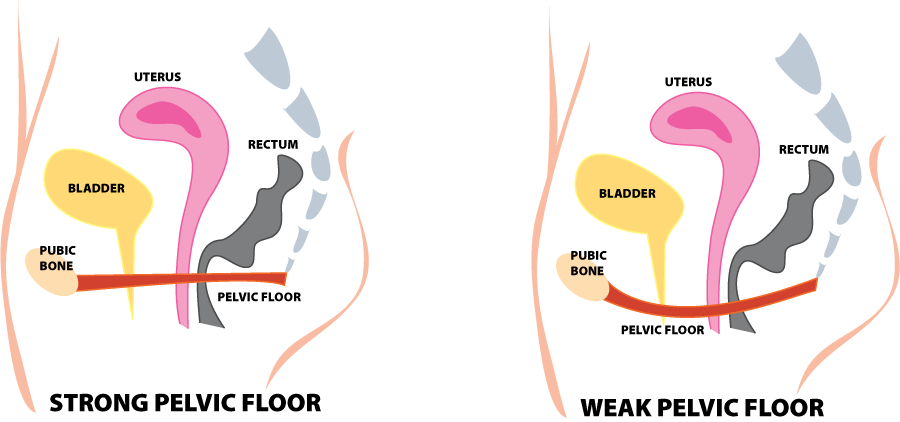
2. Pelvic Organ Prolapse
According to the International Urogynecology Association (IUGA) and the International Continence Society (ICS), pelvic organ prolapse is defined as the descent of one or more of the anterior vaginal wall, the posterior vaginal wall, the uterus (cervix) or the apex of the vagina (vaginal vault or cuff after hysterectomy). POP can be caused by a variety of circumstances including vaginal childbirth, increased age and/or BMI, increased abdominal pressure, and connective tissue disorder. The symptoms of pelvic organ prolapse (POP) include:
- Many women are asymptomatic
- The sensation of pressure or heaviness in the vagina
- Feeling of bulging or something coming out of the vagina
- Urinary symptoms: incontinence, position change or manual reduction of prolapse needed to initiate or complete voiding, weak or prolonged stream, incomplete emptying, obstructed voiding symptoms
- Bowel symptoms: incontinence, feeling of incomplete emptying, straining, digital evacuation, splinting of vagina or perineum to aid emptying
- Sexual symptoms: decreased lubrication, sensation, arousal, or dyspareunia
How physical therapy can help pelvic organ prolapse patients:
- Pelvic floor muscle training (recommended as the first line of treatment in stage 1-2 of pelvic organ prolapse)
- Strength and endurance training of underactive pelvic floor
- Stretching and relaxation of an overactive pelvic floor
- Lifestyle modification to reduce the effect of increased abdominal pressure on the pelvic organ support system
In addition to physical therapy, other treatments for POP may include pharmacological treatment, the use of mechanical devices, and surgical intervention.
3. Post Partum Recovery and/or Pain
Birthing a baby is a joyful and yet very traumatic experience. Regardless of the method of delivery, whether VBAC or Cesarean Section, each birth comes with its own potential postpartum problems. From urinary incontinence to pelvic pain, there are just some things after childbirth that are not glamorous and can be embarrassing
to discuss.
While some issues will resolve over time, there may be treatments that can help. Pelvic health physical therapy can address diastasis recti (a tear in the
abdominal wall), urinary incontinence, low back/ pelvic girdle/hip pain, pain with intercourse, or scar pain to name a few postpartum unpleasantries that may benefit from physical therapy.
Potential postpartum problems that can be helped with physical therapy:
- Urinary incontinence
- Pain with intercourse
- Pelvic floor pain
- Scar pain
- Diastasis recti
- Pelvic organ prolapse
- Difficulty returning to exercise
If you find yourself 6 weeks postpartum and still suffering, please discuss with your OB-GYN and decide if a referral to physical therapy may help.
4. Urinary Incontinence
Urinary incontinence can be embarrassing but it doesn’t have to be part of your life. Do you have to change pads every couple of hours? Do you worry
about going out because you need to know where the closest bathroom is? Do you always carry a change of clothes with you? Do you not travel or exercise because of fear of leakage? Don’t live in fear of urinary leakage.
Symptoms of Urinary Incontinence Include:
- Involuntary loss of urine
- Increased daytime/ nighttime frequency
- Urgency
- Post voiding retention
- Straining to avoid dribble
- Leakage with efforts like coughing or other activities.
How physical therapy can help urinary incontinence patients:
- Behavioral interventions (urge suppression techniques, dietary modifications, appropriate fluid intake, weight loss, habit training)
- Pelvic muscle re-training (for overactive) as well as underactive pelvic floor
- Bladder training (bladder diary or scheduled voiding)
- Neuromuscular re-education (NMES) and biofeedback devices
What to expect during a women’s health physical therapy session:
Each person will be individually evaluated and treated in a quiet, private, safe space. The initial evaluation may include an internal exam if the patient is comfortable in order to properly assess the patient’s musculature and symptoms.
- Musculoskeletal assessment: An evaluation to identify causes of poor postural alignment, strength, flexibility and movement patterns which cause orthopedic pain Soft Tissue Mobilization – to release adhesional restrictions.
- Observation and palpation of the pelvic floor to the patient’s comfort level
- Stretching and strengthening techniques
- Relaxation techniques
- Soft tissue and joint mobilization
- Modalities: Interferential electrical stimulation, ultrasound, heat or cold therapy.
- Biofeedback: Provides measurable assessment of the pelvic floor muscles ability to contract and relax in function.
- Behavior modification
- Educational instruction: Home exercise programs and information concerning diet, sleep, work and rest positions and self-management of symptoms.
If you find yourself in need of women’s health physical therapy, talk to your doctor or physical therapist and see if physical therapy would be a good fit for your symptoms. To find a physical therapist near you visit our Find A PT page.

Contributions to this blog post were provided by Spring-Klein Physical Therapy (Spring, TX), Therapy Partners of North Texas (North Richland Hills), and STAR Physical Therapy (65 locations throughout TN)

![]()