Periodization is an important technique utilized with training in order to maximize gains, whether it be through increased aerobic performance, speed, and strength. This guide outlines simple tips customizing training programs to prevent plateauing with training and improve performance. By no means is this an exhaustive guide, or an end all be all in regards to what specific exercises to perform to improve function or performance. For specifics on what exercises to perform, this depends on what goals you seek to achieve and physical characteristics, which can be outlined by a physical therapist or certified strength and conditioning coach.
1. Strength, endurance, hypertrophy, power continuing and rest
The amount of resistance, number of repetitions, and speed the exercises are performed all have an impact on how the body will respond to training. Proper training requires proper rest between sets to maximize the effect of whatever you are trying to accomplish. For a rough and dirty guide on training loads and adaptations, use the following:
Brute Strength
100% of Max (1-5 Reps)
In this range, gains are made more from neuromuscular adaptations with little effect on muscle fiber size.
REST: When training for maximum strength or power, rest for 3— 5 minutes between sets.
Power Training (High Velocity)
80-90% of Max (1-3 Reps)
At a high velocity to promote endurance and power.
REST: When training for maximum strength or power, rest for 3— 5 minutes between sets.
Strength and Mass
76-82% of Max (6-8 Reps)
This range still heavily taxes the neuromuscular system but provides a high enough volume to help elicit gains in muscle mass.
REST: When training for strength, utilize a rest scheme of 2— 3 minutes between sets.
Mass
68-74% of Max (9-12 Reps)
This range is the best for providing a high enough volume to elicit large gains in muscle mass, but not enough of a stimulus to cause as great of a strength gain as high resistances.
REST: When training to maximize muscle mass, utilize a rest scheme of 60— 90 seconds between sets.
Endurance Training
13+ REPETITIONS- These rep ranges do a better job at promoting muscular endurance, but do not have a high enough intensity to elicit large changes in muscle mass.
REST: When training for endurance, utilize a rest scheme of 30— 45 seconds between each sent.
*Note the above information is applicable to multi-joint movements like squats and deadlifts. Single joint movements, such as bicep curls, can typically be done for a greater number of repetitions at any percentage of an individual’s given maximum, and so, will need to be assessed accordingly when developing a training program.
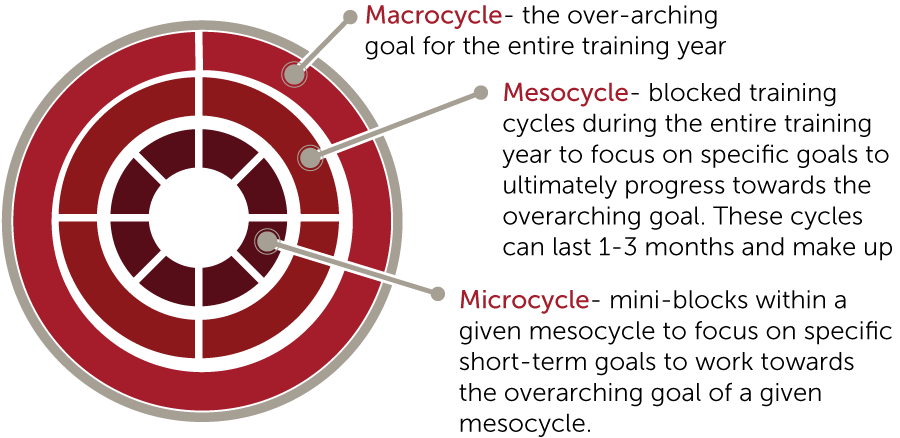
2. Training Cycles
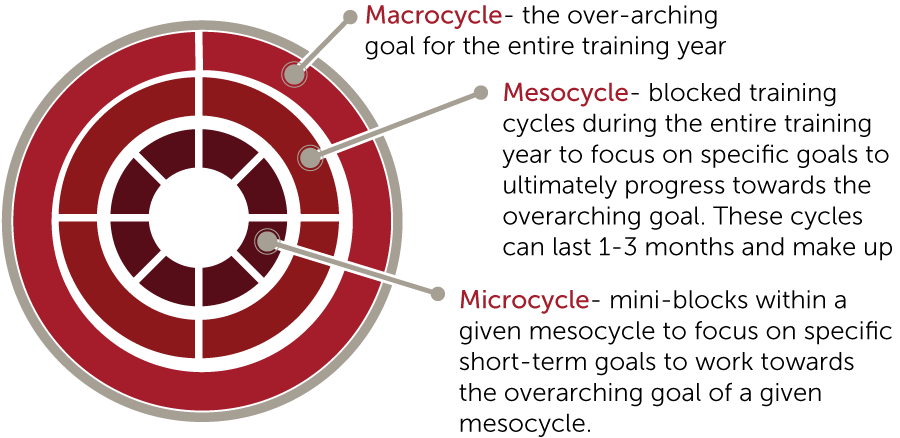
Training cycles are an organized way to design a training program to meet a specific over-arching goal. This consists of macrocycles, mesocycles, and microcycles.
3. Progressive vs. an Undulating Program
Progressive programs revolve around a systematic increase in volume, intensity, or both in a given cycle while an undulating program utilizes a randomized progression within a cycle, in which the volume, intensity, or both can vary daily, weekly, or monthly. Neither progression displays a significant superiority over one another in regards to peak performance. However, some suggest that undulating programs carry a smaller risk of overtraining. In reality, the utilization of both progression techniques allows progression and reduces the risk of overtraining while reducing the risk of plateauing.
Putting it all together (Example: 3 Month Training Progression)
Month 1- Capacity Building
Higher rep range to help the body become accustomed to training. Utilizing a combination of periodization an undulation in a month progression:
Example:
- wk 1— 4 sets of 13—15 reps at 55% — 60%;
- wk 2— 4 sets of 11—13 reps at 64%—70%;
- wk 3— 4 sets of 10—12 reps at 68%—72%;
- wk 4— 4 sets of 10—12 at 60% — 64%
Each week the rep ranges decreased with increasing resistance until week 4. The 1st 3 weeks utilize a linear progression in order to increase the body’s ability to handle a given training volume, but week 4 acts as a deloading week. This takes the undulating approach into account to alter load parameters to allow for recovery within a training cycle in order to reduce the risk of overtraining. Another important note, the higher the resistance, the lower the number of repetitions performed.
Month 2- Hypertrophy Phase
Utilize a weight that is challenging for 9 to 12 repetitions with eventually progressing to 8 to 10 repetitions utilizing progressive system detailed in month 1.
Example:
- wk 1— 10 to 12 reps at 68%— 72%
- wk 2— 9 to 11 reps at 70%— 74%
- wk 3— 8 to 10 reps at 72%— 76%
- wk 4— sets of 8 at 64%— 70%
Month 3- Strength Phase
Utilizing resistance that is challenging for 6 to 8 reps and eventually progressing to a resistance that only allows for performing 4 to 6 reps.
Example:
- wk 1— 6 to 8 reps at 76%— 82%
- wk 2— 5 to 7 reps at 78%— 85%
- wk 3— 4 to 6 reps at 82%— 88%
- wk 4 sets of 5 to 8 at 70%— 75%
This would training progression could be used a stand-alone training progression, or as part of a more comprehensive training program. The three-month block could act as a mesocycle for a larger training program with each month acting as a microcycle to address short term goals.
*Note this is by no means an exhaustive list, nor is this a specific training progression for different sports. This is just an example of how the different concepts are written in this paperwork together in a training progression.

This article was written by Rehab Associates of Northern Virginia. Rehab Associates of Central Virginia is an outpatient physical therapy clinic that focuses on putting the patient’s needs first. Their physical therapists have advanced degrees in specialty orthopedic care from head to toe.