Congratulations! You have just brought home a new bundle of joy. Now it is time for feeding every two hours, diapers, little sleep, and a flurry of casseroles and visitors. It is so easy for mom to forget to take care of herself.
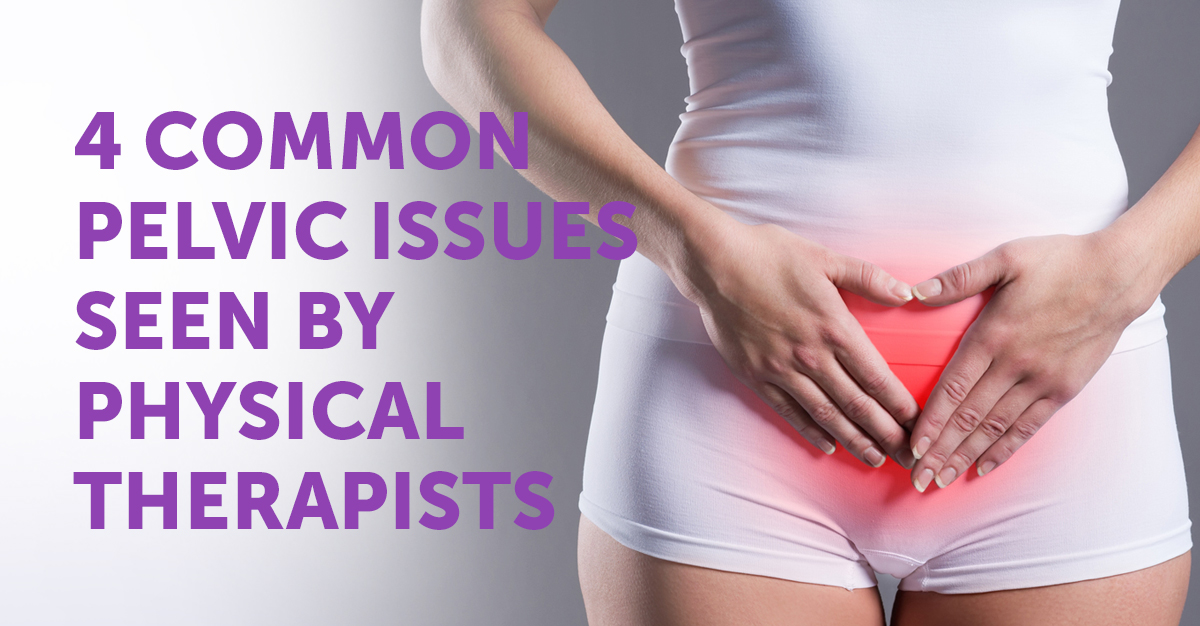
Research shows that there are a number of processes that occur in the body after giving birth that make it important to focus on maternal nutrition, exercise, mental health, and physical recovery (Walker & Grobe, 1999; Wilcox et al., 2018). For example, gestational weight gain is normal but can present a challenge when the weight is hard to lose after delivery. That extra weight can be stressful to the mom and can actually lead to additional mental and physical health issues in the future (Cuco, et al, 2006). Pelvic pain is another stressful side effect of giving birth. Understanding your postpartum pelvic pain is extremely important to your recovery as a new mom. This type of pain is very normal to experience as your pelvic bones expand and loosen while preparing your body to give birth. In turn, this expansion will make your ligaments much looser, especially after birth. More than a third of women end up with pelvic floor disorders which can lead to other serious issues that should be checked out by your doctor.
Following a physician-approved exercise plan and making necessary lifestyle changes can have a beneficial effect on both the mom and the baby as energy increases, moods stabilize, and physical activity becomes less taxing. In addition, a diet that targets low sugar and beneficial fats can reduce inflammation and improve both the recovery from childbirth and the nutritional value of breast milk (Raffelock, 2003).
While a woman is pregnant, there are specific changes in hormones that allow for the development of the baby’s skeleton and structures. As many moms-to-be can tell you, there are often visible changes in her hair, nails, and teeth that suggest a shift of her chemistry to help the baby form correctly (Gonzalez-Jaranay, et al., 2017). In fact, there are pretty specific changes in the bone density and the balance between bone degradation and bone repair (Gulson, Taylor, Eismen, 2016). While many of these processes reverse naturally after childbirth, some women (5-37% of all new moms) continue to experience poor posture, low back pain, and general muscle weakness (Bivia-Roig, 2018; Ferreria & Alburquerque-Sendin, 2013). Physical therapists can assess the problem and then create goals that focus specifically on the activities of a new mother.
Some states requires a physician’s prescription for starting physical therapy but many states now have some form of direct access where no prescription is needed. You can search for a local physical therapist by going to PT&Me.com and entering your zip code. Maternal health supports baby health. Take the time today to care for new moms
References:
Bivia-Roig G, Lison JF, Sanchez-Zuriaga D. Changes in trunk posture and muscle responses in standing during pregnancy and postpartum. 2018;13(3): 10.1371/journal.pone.0194853
Cuco G, Fernandez-Ballart J, Sala J, Viladrick C, Iranzo R. Dietary patterns and associated lifestyles in preconception, pregnancy and postpartum. European Journal of Clinical Nutrition 2006;60(3):364-71.
Gonzalez-Jaranay M, Tellez L, Rao-Lopez A, Gomez Moreno G, Moreu G. Periodontal status during pregnancy and postpartum. PLoS One 2017;12(5): doi:http://dx.doi.org.ezproxy.brenau.edu/10.1371/journal.pone.0178234
Gulson B, Taylor A, Eisman J. Bone remodeling during pregnancy and post-partum assessed by metal lead levels and isotopic concentrations. Jrnl Bone. 2016;5(5): https://doi-org.ezproxy.brenau.edu:2040/10.1016/j.bone.2016.05.005
Rafflelock D. Pregnancy and postpartum nutrition. Total Health2003;25(3):3.
Walker LO, Grobe S. The construct of thriving in pregnancy and postpartum. Nurs Science Quart. 1999;12(2): 151-157.
Wanderley C, Ferreria S, Alburquerque-Sendin F. Effectiveness of physical therapy for pregnancy-related low back and/or pelvic pain after delivery: A systematic review. Physiotherapy Theory and Practice. 2013;29(6):419-431.
Wilcox S, Jihong Liu C, Turner-McGrievy A, Burgis J, Wingard E, Dahl A, Whitaker M, Schneider L, Boutte A. A randomized controlled trial to prevent excessive gestational weight gain and promote postpartum weight loss in overweight and obese women: Health in pregnancy and postpartum (HIPP). Contemporary Clinical Trials 2018;66:51-63.