Physical Therapy for Low Back Pain: Finding Relief
Low back pain affects nearly everyone at some stage of life and is one of the most common ailments seen in medical practices. It is referred to by many different names including lumbago, lumbar sprain or strain, slipped or bulging disc, degenerative arthritis, or, when it extends into the leg, sciatica. Research suggests that between 60% – 75% of the population who experience back pain once will experience recurring or chronic problems. Most patients will not consult their physician for first-time problems with their back, so you may be one of the thousands worldwide who continue to have recurring problems with their back.
To most people, their low back pain is confusing and frustrating. Many times it starts without warning and for no obvious reason. It will interfere with the performance of basic daily activities and the ability to get a good night’s sleep. Then, often the pain will subside just as unexpectedly as it started. When in acute pain, most people are unable to think clearly about the trouble and simply seek pain relief. When episodes of back pain subside, most will then go on to forget about their back trouble. Due to a lack of understanding of the specific nature of the back problem, we are unable to deal with the problem ourselves and are unable to prevent future episodes.
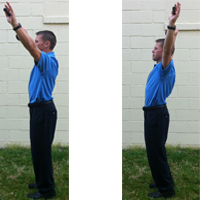
The majority of back pains are mechanical in nature, meaning that they are caused by problems with the moving parts of the spine. Therefore, certain movements that you make and positions you adopt can lead to the onset or worsening of pain. A very common example of this is patients who complain of worsening pain from bending forward for prolonged periods. Also, sitting for prolonged periods at work or while driving will bother these individuals and they might find it hard to get up from a sitting position. In some cases, it might even take a few minutes to be able to stand upright properly.
If you are like most patients with mechanical low back pain, you are better when you can move around frequently and worse when you have to remain in one position for long periods. You feel better when you are walking or are able to change positions frequently. There are times in the day when you will be much better and might even have no pain at all, and there are times when it is much worse. There are some whose pain will have worsened to the point that it is constant and the changing of positions is necessary to simply find some relief from the pain.
If you are a back pain sufferer, be encouraged that most patients can get significant help with their back pain. Exercise and activity need to be a regular part of your management strategy, but the exercise must be specific to your problem. Your program should include a daily walking program if possible. Management of your back problem is each individual’s responsibility, but we are here to help you. You may benefit from an individualized consultation with a physical therapist with specific training to evaluate mechanical spine disorders if your pain does not subside.
Common Back Problems Seen by Physical Therapists:
- Strains & Sprains
- Herniated Discs
- Degenerated Discs
- Sciatica
- Piriformis Syndrome
- Spondylosis
- Spondylolisthesis
Physical Therapy Low Back Pain Quick Assessment
If 3 or more Yes’s are present then the patient would likely benefit from a Mechanical Diagnosis and Physical Therapy Examination.
The more YESs that are present, the higher the probability of a successful outcome with a mechanical examination.
- Are symptoms present for less than 16 days in the most recent exacerbation? Yes or No
- If the patient has lower extremity symptoms, are the symptoms above the knee? Yes or No
- Does the patient’s low back pain vary in intensity? Yes or No
- Do movements or positions change the patient’s symptoms? Yes or No
- Does the patient have a hard time standing after sitting? Yes or No
- Are the symptoms worse after bending, stooping, or sitting? Yes or No
- Are the symptoms usually worse in the morning? Yes or No

For more information about physical therapy low back pain see the links below: