Soccer is a great way to build endurance, improve speed, and stay fit, all while enjoying being a part of a team. However, it does not come without it’s risks. By regularly performing quick, complicated movements combined physical contact, injuries can range from mild sprains and strains – to those that may require surgery like a torn ACL. Risk of injury is no reason not to play soccer, though. Soccer players just need to be aware of the risks and know what steps they can take to play as safely as possible.
1. Sprains
Sprains are common soccer injuries. They often happen to the ankle or knee. The pivoting and lateral movements of soccer contribute to these injuries. To avoid unnecessary risk, always check the condition of the field before you play. Do not play on fields that are uneven or have holes or rocks on them. Also, proper footwear and appropriate strength and balance training are the key to prevention.
2. Strains
Muscle strains can be caused by:
- Pulling a muscle too far in a direction it does not want to go
- Contracting a muscle hard against resistance
- Contracting a muscle hard when the muscle is not ready
The most common muscle strains in soccer occur with groin muscles, hamstrings, and quadriceps. A muscle strain won’t send you to the emergency room, but it can be painful and can keep you off the field for a few days or weeks. Strains occur frequently in soccer due to constant stop and go movement, or taking a longer stride than muscles can handle. Good flexibility and strength can lower your chances of muscle strain. Start with a warm up, then stretch the areas that are most likely to suffer a strain. Make sure that you are also doing strengthening exercises before the season begins. Wearing well-fitted cleats with appropriate spikes (longer spikes in softer turf and shorter spikes on dry, hard turf) may also help prevent strains.
3. Fractures
The majority of soccer-related fractures are also in the lower extremities . Fractures often occur as a result of contact, so wearing protective gear like shin guards is important.
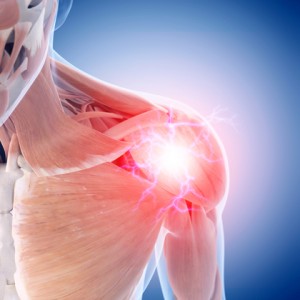
4. Head Injury
Closed-head injury is most often the result of a collision between players or from not heading the ball properly. Correct heading involves use of the forehead to contact the ball, the neck muscles to restrict head motion, and the leg muscles to to propel the body from the waist. You may want to consider strengthening your neck muscles to prepare them for heading. You can use your hand to provide resistance against your head. Then, use your neck muscles to turn your head right, left, forward, and backward. Wear a fitted mouth guard to protect your mouth and teeth. You may also want to consider protective eye-wear.
Preventing Soccer Injuries with Physical Therapy.
By working with a physical therapist for injury prevention you get the opportunity to work with an expert of the human body. A physical therapy team will be able to target specific muscles in the legs to strengthen and prepare for the movements performed regularly from athletes of all performance levels. For example, to help prevent an ACL Tear they may provide an athlete with multi directional knee stability training. In regard to head injuries a physical therapist may ask you to complete baseline testing, giving coaches and athletic trainers the ability to track your cognitive progress in case of a concussion.
Physical therapists can also help by working with teams to create more effective warm-up exercises designed specifically for your sport and ability levels.
After an Injury Occurs
If you have experienced a soccer injury that doesn’t recover after a few days of rest it may be time to consult a physical therapist or your primary health care provider. Pushing through pain while trying to remain active in a sport may lead to a more severe injury as well as improper healing of the affected muscles. By going through a physical therapy program, athletes are not only given all of the tools needed to recovery from the initial injury, but also the education and exercises needed to prevent injury in the future.
REFERENCES:
Asken MJ, Schwartz RC. Heading the ball in soccer: what’s the risk of brain injury? The Physician and Sportsmedicine. 1998;26(11).
Boden BP, Kirkendall DT, Garrett WE Jr. Concussion incidence in elite college soccer players. Am J Sports Med. 1998;26(2)238-41.
Metzl JD, Fleischer GR. Sports-specific concerns in the young athlete: soccer. J Pediat Care. 1999 April.
Soccer and the brain. University of Washington website. Available at: https://faculty.washington.edu/chudler/soccer.html. Accessed Accessed January 18, 2017.
Soccer injury prevention. American Academy of Orthopaedic Surgeons website. Available at: http://orthoinfo.aaos.org/topic.cfm?topic=A00187. Updated September 2013. Accessed January 18, 2017.
Soccer injury prevention. Stop Sports Injuries website. Available at: http://www.stopsportsinjuries.org/soccer-injury-prevention.aspx . Accessed January 18, 2017.