UNDERSTANDING PEDIATRIC INCONTINENCE
Bed wetting is almost as common as asthma, but it is often not discussed, even with doctors.
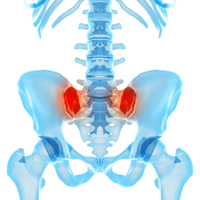
The pelvic floor is made up of muscles and other tissues that form a sling from the pubic bone to the tailbone. They help to support the abdominal and pelvic organs and assist with the control of bladder and bowel activity.
Pelvic floor dysfunction refers to a wide range of problems that occur when these muscles are weak and/or in spasm. The tissue surrounding the pelvic floor organs may have increased sensitivity and irritation or decreased sensitivity, causing the resulting dysfunction seen in children.
Although millions of children suffer from pelvic floor dysfunction, most don’t get the help they need. Typically, children are toilet trained by age 4 with only very occasional accidents. After age 4 childhood bowel and bladder dysfunction is considered a major medical problem and greatly affects quality of life for the whole family. Every day, five million American children wake up not knowing if their bed will be wet or dry. Many of these children feel embarrassed and ashamed. Bed wetting is almost as common as asthma, but it is often not discussed, even with doctors, because of its embarrassing nature.
Dysfunctional elimination in children occurs when the pelvic floor muscles are not working together with the bladder and /or bowel and the normal voiding or emptying reflexes can be disrupted. This can lead to a chronic abnormal pattern of elimination which does not allow the bladder or bowel to empty completely. Some children experience difficulty urinating or controlling their bladder function, frequent bladder infections, constipation, not urinating enough during the day, or sensing bladder fullness. Children may periodically have leakage during the day or wake up wet in the morning or both. This can be embarrassing and uncomfortable.
If your child has experienced any of the above symptoms they may have been seen by a physician or specialist, who is now recommending therapy to relax and retrain the pelvic floor muscles. Therapy can provide the tools your family needs to take control of your child’s bladder and bowel functions.
PHYSICAL THERAPY CAN HELP
If any of the below problems sound familiar, then PT can help:
• Urinary incontinence (loss of urine)
• Urinary urgency (constant/strong need to urinate)
• Urinary frequency (urinating over 8 times in a 24 hour period)
• Urinary retention (not fully emptying your bladder)
• Bed-wetting (nocturnal enuresis)
• Fecal urgency, frequency and/or retention
• Bowel incontinence, pain with defecation, inability to empty bowels
• Excessive gas, abdominal bloating
• Constipation, diarrhea with/out soiling/staining
How do we treat pediatric incontinence?
We meet with a child and their parent/s or guardian about pediatric incontinence we get a thorough knowledge of history and current problems. We then do a physical examination, looking at the muscles of the abdomen, legs, back and others we feel applicable to the specific problem. This exam is with an adult present and over clothing. Finally, we consult with the referring physician to develop an individualized treatment plan. Treatment is one-on-one, hands on, with the child dressed and lasts about one hour-in comfortable, private treatment rooms. We work with each child and family member very closely and modify our treatment according to what works best for each individual. We incorporate a holistic approach, looking at diet, sleep patterns, and other behavioral issues that could be contributing to the current problem.
What exactly do we do?
Treatment includes:
• Biofeedback-surface electromyography (external electrodes or “stickers”)
• Behavioral and diet modification
• Soft tissue mobilization, myofascial release and deep tissue massage if needed
• Hot and cold therapy
• Stretching and strengthening of pelvic floor and surrounding muscles as appropriate
• Relaxation techniques.
• Scheduled bladder retraining
• Pelvic floor muscle re-education

THE FACTS
Medical research has shown that proper pelvic floor muscle training and biofeedback drastically improves voiding dysfunctions in children.
We use animated biofeedback used a computer program with images of dolphins or space shuttle to get children to activate and relax the pelvic floor muscles.
Your child is not alone
• 20% of pediatrician visits are for incontinence problems
• 15% of visits to gastrointestinal doctors are for lower bowel dysfunction
• 3% of visits to pediatricians are for constipation
• 5 million children complain of nocturnal enuresis (nighttime bedwetting)
Common Myths
Myth: Decreasing my child’s fluid intake will decrease their incontinence?
Fact: Decreasing fluids can actually lead to dehydration, which can actually increase incontinence.
Myth: Once my child has been diagnosed with incontinence, nothing can be done about it?
Fact: Incontinence can almost always be successfully resolved, treated or managed. Physical Therapy can help!
Myth: All children gain control of their bladder and bowels at the same age?
Fact: Children develop control at different ages depending on their physical and cognitive development, as well as their environment. It is typical for a child to develop bladder and/or bowel control between two and five years of age.
HOW COMMON IS BED WETTING?
It might reassure you to know that around 19% of school-aged children wet the bed. It’s really one of the most common of all childhood problems. To give you an idea, in a class of 30 children:
Aged 5 years: 5 wet the bed at least twice a week
Aged 7 years: 2 wet the bed at least twice a week
Aged 12 years: 1 wets the bed at least twice a week
Aged 15 years: 1 child in every two classes wets the bed at least twice a week.
HEALTHY BLADDER TIPS:
1. Maintain adequate fluid intake
2. Practice prompted voiding
3. Practice bladder retraining
4. Limit intake of colas, root beer and other dark soft drinks
5. Limit caffeine intake
6. Avoid constipation
7. Exercise on a regular basis
8. Drink fluids throughout the day and limit fluids at night (2 hours before bed)
9. Keep a bladder diary