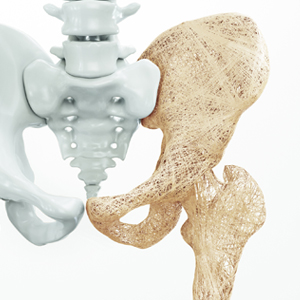
Joint pain is a common issue that can have many causes and can lead to an array of complications. Joint pain affects such a large percentage of the population. It is estimated that by the year 2030, 67 million—one in every four American adults—will have doctor-diagnosed arthritis. That doesn’t mean that we have to live in pain. It’s important to understand your pain and to take the steps needed to make sure it doesn’t lower your standard of living.
So, what are some great ways to relieve and prevent joint pain?
Going to Physical therapy
Physical therapy is a good solution for treating various joint pain symptoms. Physical therapists can help prevent or delay joint replacements, manage symptoms of arthritis/ chronic joint pain while providing tools to minimize pain or further damage to the joint, and help acutely injured joints recovery from injury. Improving flexibility and range of motion in the affected joints is also a key component in most physical therapy programs.
Getting enough movement and exercise
Even though the natural inclination for a person experiencing joint pain would be to move as little as possible, movement and light exercise will often time do the exact opposite, and be a great ally on your journey towards pain relief.
Good exercises for those who suffer from inflammation causing joint pain are aerobics, water aerobics, bicycling, burst training exercises, social activities that include movement, Tai Chi, light weight lifting, and yoga.
Go for a massage
Massaging the affected joint can be a treat, especially for joint pain occurring in the hips and knees. You can have this done at a treatment center, or have a professional who provides this type of service come to your home, but this is also something that a loved one can do for you, or that you can do yourself. An infographic from spa-hotels.ie has shown the benefits associated with massage therapy, including reducing joint pain and stress levels.
Maintain an ideal weight
Having a high BMI can cause joint pain. The more weight on the joint, the more effort is needed to move and support the body. Introducing movement and light exercise to a daily routine, as well as working towards a healthier diet, can reduce the strain on the joints. Before beginning an exercise regimen, it is important to consult your healthcare provider. A physical therapist or physician can introduce an exercise program that is tailored to your needs and ability level.
Eat an anti-inflammatory diet
Making the change to an anti-inflammatory diet is a great way to naturally alleviate joint pain. The Mediterranean diet is a good example of what anti-inflammatory eating habits should look like. One thing to be aware of is the fact that some of the most inflammatory foods out there are dairy and gluten products.
In order to mitigate joint pain through diet would be to eat a healthy amount fruits and vegetables, berries and nuts, various types of spices and herbs, as well as teas, such as green tea or ginger tea. Processed meats, fast food, artificial sweeteners, refined sugars, and chips should be cut as much as possible. Working with a nutritionist can help introduce long-term meaningful changes to a diet plan.
Get enough sleep
Believe it or not, the quality and quantity of sleep is a factor in pain relief. New research suggests that irregular sleep contributes to pain in a variety of ways, including the ability to tolerate pain. By adjusting your posture at night to keep pressure off of the painful joints, the body is able to more easily relax and allow for sleep. Exercising and remaining active throughout the day should also help you get better sleep at night.
As joint pain has become common, we tend to accept it as something we can’t really control. However, when looking at the most common causes for joint pain, we can clearly see that a sedentary lifestyle, high anxiety levels produced by stress, and unhealthy food choices are leading causes related to the issue in question.
In order to prevent inflammation, as much as in the purpose of relieving joint pain, we have to make better decisions regarding our way of living. This means creating an environment for ourselves and for our families where movement is valued and practiced on a daily basis. It also means that we should make an effort in order to ensure that there’s always a bit of time during the day to help clear one’s head by engaging in mindful practice, or by taking up a relaxing leisure activity. Equally important, it is essential to set dietary boundaries and to respect our body by not constantly abusing it with food that’s poor in nutrients, and lacks all of the advantages healthy food brings to the table when talking about the general health of the human body.