Carpal Tunnel happens when the tendons become swollen (tenosynovitis) or if the tunnel size itself decreases because of injury-causing compression to the median nerve. When compression occurs, a person can experience numbness, tingling, or a dull sensation of the thumb, index, middle and ring fingers. Symptoms may include pain during pinching and gripping, or a feeling of clumsiness and the inability to hold things. The best way to avoid carpal wrist pain is to understand the main causes of carpal tunnel and use that information at work and at home.
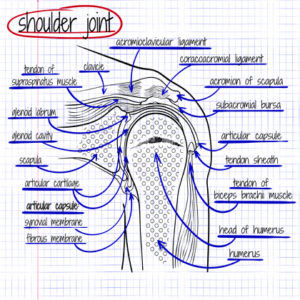
WHAT IS THE CARPAL TUNNEL?
The carpal tunnel is a small space at the wrist in which the median nerve and nine tendons pass through. The median nerve travels on top of the tendons through the tunnel. The tunnel itself is made up of your wrist bones and along the top of the tunnel is a thick fibrous ligament called the transverse carpal ligament.
COMMON CAUSES OF CARPAL TUNNEL
Carpal Tunnel is typically not related to a specific injury. Some common causes of carpal tunnel syndrome include:
Genetic Predisposition – Many cases can be a result of physical characteristics of carpal tunnel or medical conditions associated with CTS, which also run in the family.
Repetitive Movements – Certain types of work, leisure, and sports activities require use of the hand and wrist repetitively. Occupations such as manufacturing/assembly line workers, grocery checkers, musicians, carpenters, and many others require the same movements. Common hobbies such as golfing, knitting, and gardening also require repeated movements that cause carpal tunnel syndrome.
Injury or Trauma – Sprain or fracture of the wrist can cause swelling and pressure to the median nerve.
Pregnancy & Menopause – Hormonal fluctuation in women plays a role in CTS. Such fluctuation may cause fluid retention and other changes that cause swelling in the body. Fluid retention frequently occurs during the last trimester of pregnancy and is the reason for CTS.
Medical Conditions – Diabetes, hypothyroidism, lupus, obesity, and rheumatoid arthritis.

ACTIVITIES TO AVOID TO MINIMIZE SYMPTOMS
- Avoid keeping your wrists bent in either direction. The best position for the wrist is neutral (straight)
- Avoid rapid repetitive forceful or prolonged hand or arm use such as seen with factory work or data entry.
- Avoid tight gripping and pinching
- Avoid pressure to the palm or wrist
- Avoid extreme cold or vibration.