Did you know that most athletic injuries can be boiled down into three main categories? Acute, Overuse, and Chronic. Physical therapists that specialize in sports medicine, help athletes experiencing pain get back in their sport. From the time of the injury through recovery and performance, the licensed physical therapists that partner with PTandMe have the know-how and experience to get rid of your pain.


1.) ACUTE: Usually a result of a single traumatic event within the last five days. Examples: fractures, sprains, dislocations, and muscle strains.
2.) OVERUSE: Subtle and occur over time, making them challenging to diagnose and treat. Examples: swimmer’s shoulder, runner/jumpers knee, Achilles tendonitis, shin splints.
3.) CHRONIC: Usually has lasted at least three months or more.
COMMON CAUSES OF INJURIES:
- Improper training and technique
- Incorrect equipment fitting and support
- Anatomic or biomechanical issues of athlete
- Catastrophic event on or off the field

OVERUSE INJURIES AND BURNOUT
Overuse/overtraining injuries and burnout are major problems for adolescent athletes. Both can occur when students participate in sports year-round with no “off-season”, or have insufficient recovery time between practices and games.
WATCH for typical burnout signs:
- Pain during or after activity, or while at rest
- Lack of enthusiasm for practices or games
- Dip in grades
PREVENT overuse injuries and burnout with these simple tips:
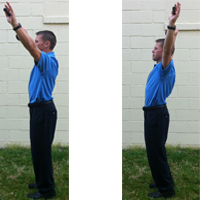
- Allow enough time for proper warm-up and cool-down routines
- Rest 1-2 days per week or engage in another activity
- Focus on strength, conditioning, or cross-training during the “off-season”
Did you know that 50% of all sports injuries to student-athletes are a result of overuse?
SPRAIN
Sprains result from overstretching or tearing of the joint capsule or ligament which attaches a bone to another bone.
STRAIN
Strains, also referred to as pulls, result from over-stretching or tearing a muscle or tendon, which attaches a muscle region to a bone.
CONTUSIONS
Contusions or bruises are an injury to tissue or bone in which the capillaries are broken and local bleeding occurs.
TEARS
Tears are a complete separation of the tissue fibers.
Physical therapy and athletics go hand in hand. In many cases, your PT may be a former athlete that experienced an injury in their youth, and as a result, found a passion for rehabilitating others. If you are experiencing pain, or have already had an injury, don’t wait to talk to your physical therapist. The faster you ask for help the faster you can get back into your sport.
For more information about physical therapy and sports medicine – try the links below:
This article about athletic injuries was provided by PTandMe physical therapy partner: The Center for Physical Rehabilitation. More information about the Center and its locations throughout Grand Rapids, MI can be found on its website at www.pt-cpr.com