Whether you are getting ready for a move, or need to lift things at work, it’s important to use safe lifting practices. Don’t end up with a hurt back – use these tips to keep yourself injury free.
• ESTABLISH A BASE OF SUPPORT: Use a wide, balanced stance with one foot in front of the other. Make sure that you have firm footing and that your feet are a shoulders-width apart. This staggered stance gives you the stability of not falling over and being able to secure the load.•
• KEEP YOUR EYES UP: Looking slightly upward will help you maintain a better position of the spine. Keeping your eyes focused upwards helps you keep your back straight.
• GET A GOOD GRIP: with your palms and make sure you have an adequate hold on the object. Be certain you will be able to maintain a hold on the object without having to adjust your grip later. You can use gloves to help maintain an adequate grip, but don’t rely on gloves because they can desensitize the fingers and make you unable to feel the object.
• LIFT GRADUALLY WITH YOUR LEGS: without using jerky motions. By using your leg strength, your chance of lower back injury is greatly reduced.
• TIGHTEN YOU STOMACH MUSCLES: as you begin the lift and keep you head and shoulders up.
• PIVOT � DON’T TWIST: Move your feet in the direction of the lift. This will eliminate the need to twist at the waist.
• WEIGHT: A lighter load normally means a lesser risk of injury. The weight of the object should be within the capacity of the person to handle safely.
• HANDLING: It is easier to pull or push a load than it is to lift, put down or carry.
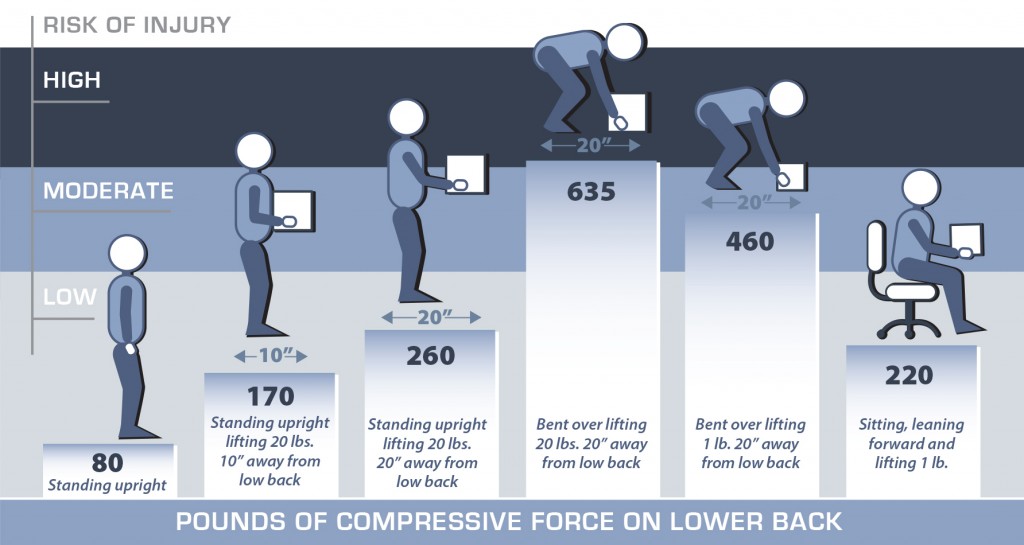
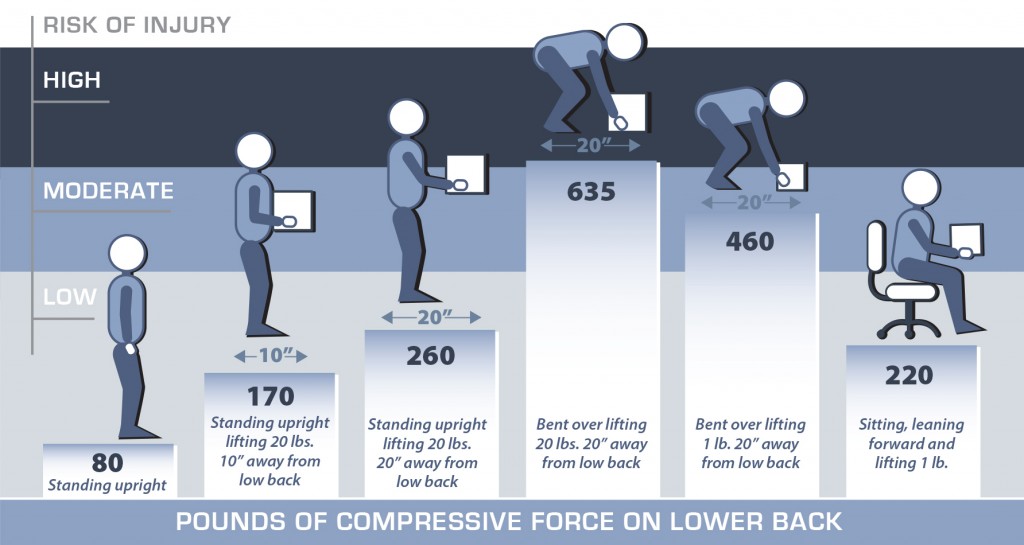
• KEEP THE LOAD CLOSE: Holding a 20 lb. object with your hands 20 inches from the body creates more compressive force on your low back than holding it 10 inches away. This is because the muscles in your back have to work to counterbalance the weight when it is further from the body. As the compressive force on your low back increases, so does the risk of muscle strains, ligament sprains and damage to the disks in the spine.
• FREQUENCY: The more times a load is handled, the more tired the muscles become, making it easier for the person to be injured.
• DISTANCE: The farther the load has to be moved, the greater the risk of injury.
• DURATION �TIME�: Where the job involves repetitive movements, reducing the time spent on handling will help to ensure the movements are not causing unnecessary strain.
• FORCES APPLIED: Forces should be applied smoothly, evenly and close to the body. Forces exerted should be well within the capacity of the person, and the person should maintain proper posture.
• NATURE OF THE LOAD: Loads that are compact, stable, easy to grip, and capable of being held close to the body are much easier to handle.
• TERRAIN: Rough ground, steep slopes, slippery and uneven floors, stairs and cluttered floors make moving a load awkward and increase the chance for injury.
• ENVIRONMENT �(CLIMATE & LIGHTING)�: If it is too hot, too humid, too cold or the lighting is inadequate, the capacity to work safely is reduced.
• CONDITION OF THE WORKPLACE: Safe and comfortable working conditions, with adequate space to perform the task, and tools and equipment that are well-maintained, make their job safer.
• AGE/GENDER: Young and old workers alike may be at an increased risk of injury from manual materials handling activities. Ensure abilities of employees are in line with functional job requirements.
• TRAINING: Proper training for the specific task is vital to reduce injury.
• TEAM LIFTING: If one person cannot lift or move a heavy, large or awkward object safely, organize a team lift. Team lifting reduces the risk of injury, reduces fatigue and makes the task much easier.
• RAISE/LOWER SHELVES: The best zone for lifting is between your shoulders and your waist. Put heavier objects on shelves at waist level, lighter objects on lower or higher shelves.
• AVOID LIFTING FROM THE FLOOR: Lifting from the floor can greatly increase your risk of injury for two reasons. Firstly, it is difficult to bring objects close to your body when picking them up from the floor, especially large objects where your knees can get in the way. Secondly, your low back must now support the weights of your upper body as you lean forward, in addition to supporting the weight of the item you are lifting. Lifting the same 20lbs from the floor more than doubles the amount of force on your low back when compared with lifting is from waist height. Even a one pound object lifted from the floor increases you risk of injury if you use a bent over posture.
• GET HELP WHEN YOU NEED IT: Don’t try to lift heavy or awkward loads on your own. Even though the muscles in your upper body may be strong enough to handle the load, the muscles, ligaments and disks in your lower back may be injured because of the additional forces they have to withstand. Get help from a co-worker, and whenever possible, use a cart, hand truck or other mechanical device to move the load for you.
PROPER LIFTING TECHNIQUE

IMPROPER LIFTING TECHNIQUE

POSTURE
GOOD POSTURE
BAD POSTURE