Definition
Glucose is a type of sugar. It comes from food, and is also created in the liver. Glucose travels through the body in the blood. It moves from the blood to cells with the help of a hormone called insulin. Once glucose is in those cells, it can be used for energy.
Diabetes is a condition that makes it difficult for the body to use glucose. This causes a buildup of glucose in the blood. It also means the body is not getting enough energy. Type 2 diabetes is one type of diabetes, and it is the most common.
Medication, lifestyle changes, and monitoring can help control blood glucose levels.
Causes
Type 2 diabetes is often caused by a combination of factors. One factor is that your body begins to make less insulin. A second factor is that your body becomes resistant to insulin. This means there is insulin in your body, but your body cannot use it effectively. Insulin resistance is often related to excess body fat.
Risk Factors
Type 2 diabetes is more common in people who are aged 45 years and older. It is also common in younger people who are obese and belong to at-risk ethnic groups. Other factors that increase your chance for type 2 diabetes include:
• Prediabetes — impaired glucose tolerance and impaired fasting glucose
• Metabolic syndrome — a condition marked by elevated cholesterol, blood glucose, blood pressure, and central obesity
• Excess weight or obesity, especially central obesity
• Lack of exercise
• Poor diet — high intake of processed meats, fats, sugar-sweetened foods and beverages, and calories
• Family history of type 2 diabetes
• High blood pressure
• History of cardiovascular disease
• Depression
• History of gestational diabetes, or having a baby that weighs over 9 pounds at birth
• Endocrine disorders, such as Cushing’s syndrome, hyperthyroidism, acromegaly, polycystic ovary syndrome, pheochromocytoma, or glucagonoma
• Conditions associated with insulin resistance, such as acanthosis nigricans
• Certain medications, such as glucocorticoids or thiazides
• Certain ethnic groups, such as African American, Hispanic, Native American, Hispanic American, Asian American, or Pacific Islander
Symptoms
You may have diabetes for years before you have symptoms. Symptoms caused by high blood sugar or include:
• Increased urination
• Extreme thirst
• Hunger
• Fatigue
• Blurry vision
• Irritability
• Frequent or recurring infections
• Poor wound healing
• Numbness or tingling in the hands or feet
• Problems with gums
• Itching
• Problems having an erection
Diagnosis
The doctor will ask about your symptoms and medical history. You will also be asked about your family history. A physical exam will be done.
Diagnosis is based on the results of blood testing. American Diabetes Association (ADA) recommends diagnosis be made if you have one of the following:
• Symptoms of diabetes and a random blood test with a blood sugar level greater than or equal to 200 mg/dL (11.1 mmol/L)
• Fasting blood sugar test is done after you have not eaten for 8 or more hours—showing blood sugar levels greater than or equal to 126 mg/dL (7 mmol/L) on two different days
• Glucose tolerance test measures blood sugar 2 hours after you eat glucose—showing glucose levels greater than or equal to 200 mg/dL (11.1 mmol/L)
• HbA1c level of 6.5% or higher—indicates poor blood sugar control over the past 2-4 months
* mg/dL = milligrams per deciliter of blood; mmol/L = millimole per liter of blood
Treatment
Treatment aims to:
• Maintain blood sugar at levels as close to normal as possible
• Prevent or delay complications
• Control other conditions that you may have, like high blood pressure and high cholesterol
Diet
Food and drinks have a direct effect on your blood glucose level. Eating healthy meals can help you control your blood glucose. It will also help your overall health. Some basic tips include:
• Follow a balanced meal plan. It should include carbohydrates, proteins, and fats.
• Be aware of appropriate serving size. Measure your food to help understand ideal serving size.
• Do not skip meals. Plan your meals and snacks through the day. Having meals throughout the day can help avoid major changes in glucose levels.
• Eat plenty of vegetables and fiber.
• Limit the amount of fat (especially saturated and trans fats) in your foods.
• Eat moderate amounts of protein and low-fat dairy products.
• Carefully limit foods containing high concentrated sugar.
• Keep a record of your food intake. Share the record with your dietitian or doctor. This will help to create an effective meal plan.

Weight Loss
If you are overweight, weight loss will help your body use insulin better. Talk to your doctor about a healthy weight goal. You and your doctor or dietitian can make a safe meal plan for you.
These options may help you lose weight:
• Use a portion control plate
• Use a prepared meal plan
• Eat a Mediterranean-style diet
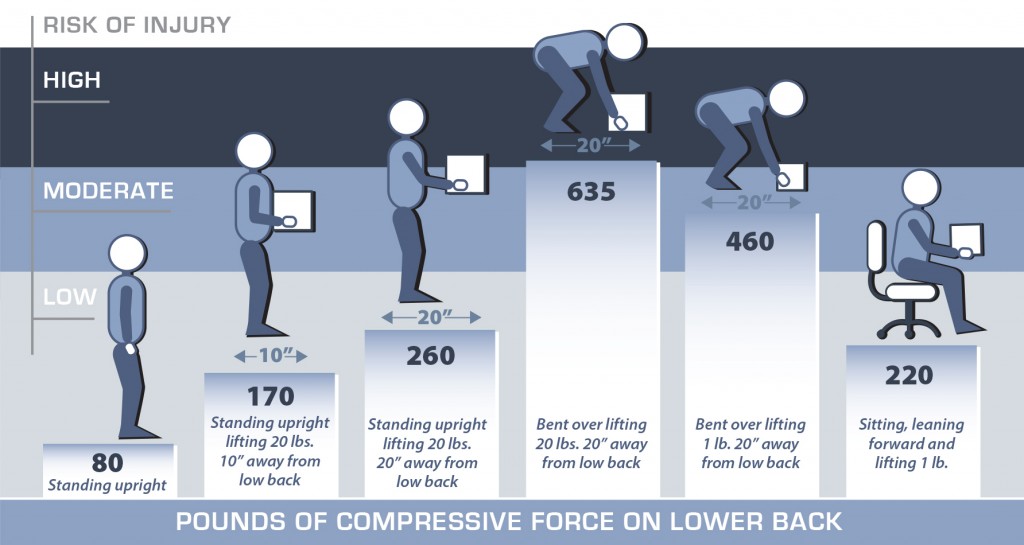
Exercise
Physical activity can:
• Make the body more sensitive to insulin
• Help you reach and maintain a healthy weight
• Lower the levels of fat in your blood
Aerobic exercise is any activity that increases your heart rate. Resistance training helps build muscle strength. Both types of exercise help to improve long-term glucose control. Regular exercise can also help reduce your risk of heart disease.
Talk to your doctor about an activity plan. Ask about any precautions you may need to take.
Medication
Certain medications will help to manage blood glucose levels.
Medication taken by mouth may include:
• Biguanides reduce the amount of glucose made by the body
• Sulfonylureas encourage the pancreas to make more insulin
• Insulin sensitizers to help the body use insulin better
• Starch blockers to decrease the amount of glucose absorbed into the blood
• Sodium-glucose co-transporter 2 (SGLT-2) inhibitors to increase glucose excretion in urine
• Bile acid binders
Some medications needs to be given by injection, such as:
• Incretin-mimetics stimulate the pancreas to produce insulin and decrease appetite, which can assist with weight loss
• Amylin analogs replace a protein of the pancreas that is low in people with type 2 diabetes
Insulin
Insulin may be needed if:
• The body does not make enough of its own insulin
• Blood glucose levels cannot be controlled with lifestyle changes and medications
Insulin is given through injections. There is one short-acting inhaled insulin which may be available for select persons.
Blood Glucose Testing
You can check the level of glucose in your blood with a blood glucose meter. Checking your blood glucose levels during the day can help you stay on track. It will also help your doctor determine if your treatment is working. Keeping track of blood sugar levels is especially important if you take insulin.
Regular testing may not be needed if your diabetes is under control and you don’t take insulin. Talk with your doctor before stopping blood sugar monitoring.
An HbA1c test may also be done at your doctor’s office. This is a measure of blood glucose control over a long period of time. Doctors advise that most people keep their HbA1c levels below 7%. Your exact goal may be different. Keeping HbA1c in your goal range can help lower the chance of complications.
Counseling
Depression can undermine your recovery and put you at risk for other complications. Feelings of sadness, hopelessness, and loss of interest in your favorite activities that stay with you for at least 2 weeks should prompt you to call your doctor. Depression is treatable. Your doctor may refer you to counseling to help you better manage your depression and diabetes.
Decreasing Risk of Complications
Over a long period of time, high blood glucose levels can damage vital organs. The kidneys, eyes, and nerves are most affected. Diabetes can also increase your risk of heart disease.
Maintaining goal blood glucose levels is the first step to lowering your risk of these complications. Other steps:
• Take good care of your feet. Be on the lookout for any sores or irritated areas. Keep your feet dry and clean.
• Have your eyes checked once a year.
• Don’t smoke. If you do, look for programs or products that can help you quit.
• Keep track of your moods and be alert for persistent depressive symptoms.
• Plan medical visits as recommended.
Prevention
To help reduce your chance of type 2 diabetes:
• Participate in regular physical activity
• Maintain a healthy weight
• Drink alcohol only in moderation (2 drinks per day for a man, and 1 drink per day for a woman)
• Eat a well-balanced diet:
– Get enough fiber
– Avoid fatty foods
– Limit sugar intake
– Eat more green, leafy vegetables
– Eat whole fruits, especially apples, grapes, and blueberries
by Debra Wood, RN
RESOURCES:
American Diabetes Association
http://www.diabetes.org
National Diabetes Information Clearinghouse
http://diabetes.niddk.nih.gov
CANADIAN RESOURCES:
Canadian Diabetes Association
http://www.diabetes.ca
Public Health Agency of Canada
http://www.phac-aspc.gc.ca
REFERENCES:
American Association of Clinical Endocrinologists, American College of Endocrinology. Medical guidelines for the management of diabetes mellitus. The AACe system of intensive diabetes self-management. 2002 update. Endocrine Practice. 2002;8(suppl 1):S40-S82.
American Diabetes Association Diagnosis and Classification of Diabetes Mellitus. Diabetes Care. 2010;33:S62-S69.
Boren SA, Gunlock TL, Schaefer J, Albright A. Reducing risks in diabetes self-management: a systematic review of the literature. Diabetes Educ. 2007;33:1053-1077.
Causes of diabetes. National Institute of Diabetes and Digestive and Kidney Diseases website. Available at: http://www.niddk.nih.gov/health-information/health-topics/Diabetes/causes-diabetes/Pages/index.aspx. Updated June 2014. Accessed September 3, 2015.
Diabetes. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/diabetes/home/index.html. Updated August 18, 2015. Accessed September 3, 2015.
Diabetes mellitus type 2 in adults. EBSCO DynaMed Plus website. Available at: http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults. Updated August 29, 2016. Accessed September 29, 2016.
Diabetes mellitus type 2 in children and adolescents. EBSCO DynaMed Plus website. Available at: http://www.dynamed.com/topics/dmp~AN~T901364/Diabetes-mellitus-type-2-in-children-and-adolescents. Updated June 9, 2016. Accessed September 29, 2016.
Diagnosis and classification of diabetes mellitus. Diabetes Care. 2005;28(suppl 1):S37-42.
Dietary considerations for patients with type 2 diabetes. EBSCO DynaMed Plus website. Available at: http://www.dynamed.com/topics/dmp~AN~T270045/Dietary-considerations-for-patients-with-type-2-diabetes. Updated January 19, 2016. Accessed September 29, 2016.
Gaede P, Vedel P, Larsen N, et al. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;248:383-393.
Harsch IA. Inhaled insulins: their potential in the treatment of diabetes mellitus. Treat Endocrinol. 2005;4:131-138.
Lee DC, Sui X, Church TS, Lee IM, Blair SN. Associations of cardiorespiratory fitness and obesity with risks of impaired fasting glucose and type 2 diabetes in men. Diabetes Care. 2009;32:257-262.
Marre M. Reducing cardiovascular risk in diabetes. J Hypertens. 2007;(supp 11)S19-22.
Physical activity/exercise and diabetes. Diabetes Care. 2004;27(suppl 1):S58-62.
Rosenbloom AL, Silverstein JH, Amemiya S, et al. ISPAD Clinical Practice Consensus Guideline 2006-2007. Type 2 diabetes mellitus in the child and adolescent. Pediatr Diabetes. 2008;9:512-526.
Rosenzweig JL, Ferrannini E, Grundy SM, et al. Primary prevention of cardiovascular disease and type 2 diabetes in patients at metabolic risk: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008;93:3671-3689.
Skyler JS, Bergenstal R, Bonow RO, et al. Intensive glycemic control and the prevention of cardiovascular events: Implications of the ACCORD, ADVANCE and VA diabetes trials: a position statement of the American Diabetes association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association. Circulation. 2009;119:351-7.
Standards of medical care in diabetes—2009. Diabetes Care. 2009;32:S13-61.
Statement by an AACE/ACE Consensus Panel on Type 2 Diabetes Mellitus: An Algorithm for Glycemic Control. Endocr Pract. 2009;15:540-559.
Traina AN, Kane MP. Primer on pramlintide, an amylin analog. Diabetes Educ. 2011;37(3):426-431.
Type 2. American Diabetes Association website. Available at: http://www.diabetes.org/diabetes-basics/type-2/?loc=HomePage-type2-tdt. Accessed September 3, 2015.
UK Prospective Diabetes Study Group. Effect of intensive blood-glucose control with metformin on complications in overweight patients with type 2 diabetes. Lancet. 1998;352:954-965.
US Preventive Services Task Force: Screening for type 2 diabetes mellitus in adults: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2008;148:846-854.
11/29/2006 DynaMed Plus Systematic Literature Surveillance.http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Lindstrom J, Ilanne-Parikka P, Peltonen M, Aunola S, Eriksson JG, Hemio K, et al. Sustained reduction in the incidence of type 2 diabetes by lifestyle intervention: follow-up of the Finnish Diabetes Prevention Study. Lancet. 2006;368:1673-1679.
9/19/2006 DynaMed Plus Systematic Literature Surveillance.http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Thomas DE, Elliott EJ, Naughton GA. Exercise for type 2 diabetes mellitus. Cochrane Database of Syst Rev. 2006;CD002968.
6/1/2007 DynaMed Plus Systematic Literature Surveillance.http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Nissen SE, Wolski K. Effect of rosiglitazone on the risk of myocardial infarction and death from cardiovascular causes. N Engl J Med. 2007;356(24):2457-2471.
7/13/2007 DynaMed Plus Systematic Literature Surveillance.http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Farmer A, Wade A, Goyder E, et al. Impact of self-monitoring of blood glucose in the management of patients with non-insulin treated diabetes: open parallel group randomised trial. BMJ. 2007;335(7611):132.
12/13/2007 DynaMed Plus Systematic Literature Surveillance.http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Milman U, Blum S, Shapira C, et al. Vitamin E supplementation reduces cardiovascular events in a subgroup of middle-aged individuals with both type 2 diabetes mellitus and the haptoglobin 2-2 genotype. A prospective double-blinded clinical trial. Arterioscler Thromb Vasc Biol. 2008;28(2):341-347.
2/28/2008 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Davies MJ, Heller S, Skinner TC, et al. Effectiveness of the diabetes education and self management for ongoing and newly diagnosed (DESMOND) programme for people with newly diagnosed type 2 diabetes: cluster randomised controlled trial. BMJ. 2008;336(7642):491-495.
2/28/2008 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Christian JG, Bessesen DH, Byers TE, Christian KK, Goldstein MG, Bock BC. Clinic-based support to help overweight patients with type 2 diabetes increase physical activity and lose weight. Arch Intern Med. 2008;168:141-146.
6/18/2008 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358:2560-2572.
2/24/2009 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Liese AD, Weis KE, Schulz M, Tooze JA. Food intake patterns associated with incident type 2 diabetes: the Insulin Resistance Atherosclerosis Study. Diabetes Care. 2009;32:263-268.
5/11/2009 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Loimaala A, Groundstroem K, Rinne M, et al. Effect of long-term endurance and strength training on metabolic control and arterial elasticity in patients with type 2 diabetes mellitus. Am J Cardiol. 2009;103:972-977.
8/19/2009 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Li TY, Brennan AM, Wedick NM, Mantzoros C, Rifai N, Hu FB. Regular consumption of nuts is associated with a lower risk of cardiovascular disease in women with type 2 diabetes. J Nutr. 2009;139:1333-1338.
10/12/2009 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Crandall JP, Polsky S, Howard AA, et al. Alcohol consumption and diabetes risk in the Diabetes Prevention Program. Am J Clin Nutr. 2009;90:595-601.
11/20/2009 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Lund SS, Tarnow L, Frandsen M, et al. Combining insulin with metformin or an insulin secretagogue in non-obese patients with type 2 diabetes: 12 month, randomised, double blind trial. BMJ. 2009;339:b4324.
12/21/2009 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Cappuccio FP, D’Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(2):414-420.
2/15/2010 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: American Diabetes Association. Standards of medical care in diabetes—2010. Diabetes Care. 2010;33(suppl 1:S11-61).
2/15/2010 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(suppl 1:S62-69).
7/2/2010 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Micha R, Wallace SK, Mozaffarian D. Red and processed meat consumption and risk of incident coronary heart disease, stroke, and diabetes mellitus: a systematic review and meta-analysis. Circulation. 2010;121(21):2271-2283.
10/5/2010 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Carter P, Gray LJ, Troughton J, Khunti K, Davies MJ. Fruit and vegetable intake and incidence of type 2 diabetes mellitus: systematic review and meta-analysis. BMJ. 2010;341:c4229.
1/4/2011 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Pan A, Lucas M, Sun Q, et al. Bidirectional association between depression and type 2 diabetes mellitus in women. Arch Intern Med. 2010;170(21):1884-1891.
5/6/2011 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Muraki I, Imamura F, Manson J, et al. Fruit consumption and risk of type 2 diabetes: results from three prospective longitudinal cohort studies. BMJ. 2013;347:f5001.
4/14/2014 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Xi B, Li S, et al. Intake of fruit juice and incidence of type 2 diabetes: a systematic review and meta-analysis. PLoS One. 2014;9(3):e93471.
7/21/2014 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Afshin A, Micha R, et al. Consumption of nuts and legumes and risk of incident ischemic heart disease, stroke, and diabetes: a systematic review and meta-analysis. Am J Clin Nutr. 2014;100(1):278-288.
9/11/2014 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Tovote KA, Fleer J, Snippe E, et al. Individual mindfulness-based cognitive therapy and cognitive behavior therapy for treating depressive symptoms in patients with diabetes: results of a randomized controlled trial. Diabetes Care. 2014;37(9):2427-2434.
9/16/2014 DynaMed Plus Systematic Literature Surveillance http://www.dynamed.com/topics/dmp~AN~T113993/Diabetes-mellitus-type-2-in-adults: Zhou D, Yu H, He F, et al. Nut consumption in relation to cardiovascular disease risk and type 2 diabetes: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr. 2014;100(1):270-277.
Last reviewed January 2016 by Kim Carmichael, MD
EBSCO Information Services is fully accredited by URAC. URAC is an independent, nonprofit health care accrediting organization dedicated to promoting health care quality through accreditation, certification and commendation.