Hypertension is abnormally high blood pressure. High blood pressure puts extra strain on the heart, lungs, brain, and kidneys. It carries with it an increased risk of death and disability from coronary artery disease (CAD), stroke, heart failure, and kidney disease.
High blood pressure is very common but can’t be seen or felt. Many people with high blood pressure don’t know they have it. The best way to know if you have high blood pressure is to keep track of your numbers. You can get your blood pressure checked at your doctor’s office, at home, or at your local pharmacy. It’s important to get your blood pressure checked regularly.
Defining High Blood Pressure
High blood pressure is defined by 2 numbers (systolic and diastolic). The systolic or top number measures the pressure in your blood vessels when your heart beats. The diastolic or bottom number measures the pressure in your blood vessels when your heart rests between beats.
The normal blood pressure varies with age, usually increasing as we get older. In general, systolic blood pressure (SBP) less than 120 mm Hg and diastolic blood pressure (DBP) less than 80 mm Hg are considered normal and prehypertension is a SBP120-139 mm Hg or DPB 80-89 mm Hg. Abnormal levels include:
• Stage 1 hypertension—SBP 140-159 mm Hg or DPB 90-99 mm Hg
• Stage 2 hypertension—SBP more than 160 mm Hg or DBP more than 100 mm Hg
In people with diabetes or kidney disease, the targets numbers are lower. Check with your doctor to see what your target range should be.
Common Risk Factors
There is no single cause for high blood pressure, but there are several factors that can increase your risk.
Some risk factors for high blood pressure include:
• Age: middle-aged or elderly—onset generally happens at 20-50 years, but likelihood increases with age
• Race: African American
• Gender: Male
Medical factors, such as:
• Diabetes
• Obesity
• Metabolic syndrome—A condition marked by elevated blood pressure, cholesterol, blood glucose, and body weight. Excess weight centered around the midsection is of particular concern.
• A family history of high blood pressure
• Sleep apnea
• Prehypertension
Lifestyle factors, such as:
• Smoking
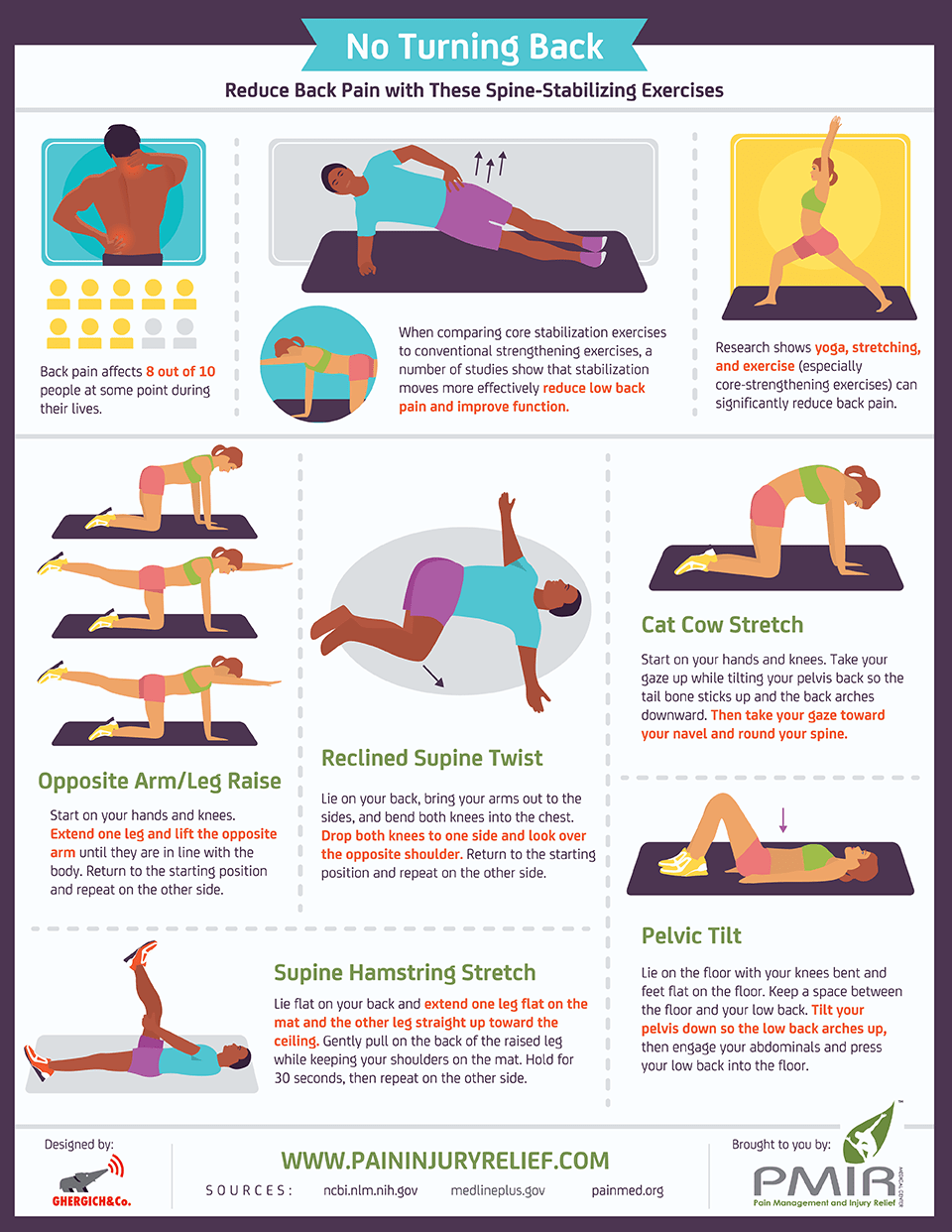
• Being physically inactive
• Taking birth control pills
• Having diet high in red meat, salt, and saturated and trans fats
• High alcohol intake
Risk factors don’t mean you will get high blood pressure, but that you have an increased chance of developing it. Fortunately, there are also factors that can help you prevent high blood pressure or lower your blood pressure if you already have elevated blood pressure.

Lifestyle Guidelines to Prevent or Reduce High Blood Pressure
The National Heart, Lung, and Blood Institute’s recommendations to help prevent or lower high blood pressure include:
• Losing weight if you are overweight
• Increasing levels of physical activity—Aim for 30 minutes per day on most days of the week.
• Eating a diet rich in fruits, vegetables, and low-fat dairy products
• Eating a diet that is low in saturated and total fat
• Limiting consumption of sodium (salt) to less than 2,300 milligrams per day
• Drinking alcohol only in moderation—This means 1 drink or less per day for women and 2 drinks per day or less for men.
Another approach endorsed by National Heart, Lung, and Blood Institute is use of the DASH diet. This is a special low-salt diet which has been shown effective in both preventing and treating high blood pressure.
High blood pressure is a major player in heart disease and stroke. Protect yourself and know your numbers. The next time you take a trip to the pharmacy, check your blood pressure. If you do it on a regular basis and follow the lifestyle guidelines, you may be able to avoid future problems.
by Michael Jubinville, MPH
RESOURCES:
National Heart, Lung, and Blood Institute
https://www.nhlbi.nih.gov
American Heart Association
http://www.heart.org
CANADIAN RESOURCES:
Health Canada
http://www.hc-sc.gc.ca
Heart & Stroke Association
http://www.heartandstroke.ca
REFERENCES:
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension. 2003;42(6):1206-1252.
How can high blood pressure be prevented? National Heart Lung and Blood Institute website. Available at: http://www.nhlbi.nih.gov/health/health-topics/topics/hbp/prevention. Updated September 10, 2015. Accessed August 2, 2016.
Hypertension. EBSCO DynaMed website. Available at: http://www.ebscohost.com/dynamed. Updated July 12, 2016. Accessed August 2, 2016.
Hypertension treatment in patients with diabetes. EBSCO DynaMed website. Available at: http://www.ebscohost.com/dynamed. Updated April 11, 2016. Accessed August 2, 2016.
Preventing high blood pressure: Healthy living habits. Centers for Disease Control and Prevention website. Available at: http://www.cdc.gov/bloodpressure/what_you_can_do.htm. Updated July 7, 2014. Accessed August 2, 2016.
Understanding your risk for high blood pressure. American Heart Association website. Available at: http://www.heart.org/HEARTORG/Conditions/HighBloodPressure/UnderstandYourRiskforHighBloodPressure/Understand-Your-Risk-for-High-Blood-Pressure_UCM_002052_Article.jsp#.V6CgG02FPIU. Updated June 29, 2016. Accessed August 2, 2016.
Whelton PK, He J, Appel LJ, et al. Clinical and public health advisory from the National High Blood Pressure Education Program. JAMA. 2002;288(15):1882-1888.
Last reviewed July 2016 by Michael Woods, MD Last Updated: 8/2/2016
EBSCO Information Services is fully accredited by URAC. URAC is an independent, nonprofit health care accrediting organization dedicated to promoting health care quality through accreditation, certification and commendation.